I first developed an interest in genitourethral reconstruction, particularly urethroplasty, at the beginning of my urology training. Working in Bristol and Weston Super Mare for David Dickerson inspired me to develop this further. Mr Dickerson performs one of the largest volume of urethroplasties in the UK and it was a privilege to work for him.
I was quite junior at the time and so my experience was largely as first assistant but I learnt a huge amount about the management of urethral stricture disease; both operatively and perhaps more importantly the decision- making about whether to operate and the thinking behind what operation to perform. Mr Dickerson is also the supra-regional lead for penile cancer in the South West and so I was able to gain some exposure to this as well. To me it seems very logical that penile cancer surgery and genitourethral reconstruction should go together although I know that in many UK centres penile cancer is managed by andrologists.
Being the sole surgeon performing genitourethral reconstructive surgery in the South West for more than 20 years, Mr Dickerson was keen that any new member of the team went away and learnt new techniques and gained new experience which could be brought back to the region. I went on to complete my urology training, gaining exposure to all sub-specialities of urology including robotics which seems to be a favourite amongst trainees, although not for me! Despite this, I could not get away from my first love of urethroplasty. I maintained some continuity with genitourethral surgery during my rotations, including a visit with Urolink to Moshi, Tanzania in 2013. Following this I published a report in Urology News about my experience (May/June 2014 issue).
“On top of the excellent clinical experience in St George’s and Epsom, I was able to take part in management roles, clinical research, teaching and also assisting in the private sector.”
Once my FRCS(Urol) exam was out of the way in May 2015, I focused on fellowship planning and getting my CCT. I’d heard great things about fellowships in Australia, particularly the volume of surgical experience, so in fact I had initially organised a fellowship in Sydney. This was a very general fellowship with a small amount of exposure to urethroplasty. In the end it turned out this fellowship was not right for me or my family so I pulled out. In October 2015 I was starting my ST7 year and was keen to get things organised so I knew what I would be doing once I had finished. I had further discussions with Mr Dickerson and my boss at the time Edward Rowe, and they both suggested getting in touch with Nick Watkin at St George’s Hospital in London. I knew of Nick Watkin and had read his name many times in publications on penile cancer and urethral surgery but we had never met. I also knew the person who was currently working with him so making contact did not seem too daunting. My aim was always to return to the South West and it became apparent that there was a need for an additional surgeon. So I took on board Mr Dickerson’s advice and made plans to go and learn new skills that would be useful if I was to return. This included, for example, dynamic sentinel node sampling for penile cancer which is not currently performed for penile cancer in Bristol.
Organising the fellowship
Having spoken to Wayne Lam, who was working for Mr Watkin at the time, I realised this would be a great opportunity to develop and learn new skills. With young children and a wife who is medical I had to consider them in my big plans. When we were intending to go to Sydney we had worked it out; my wife would have a year off and we would be together. Moving to London, however, proved to be more challenging. Since my wife and children were set up in Bristol we decided that they would stay and I would spend the week in London and commute back at weekends. This was tough, more so for my wife, but I missed a lot of time with my children.
In September 2015, just over a year before I was due to finish my training, I emailed Mr Watkin. Very promptly he replied thanking me for my interest and after further email exchanges about what I could expect from the fellowship we arranged to meet. I made the trip to Epsom, where Mr Watkin also works, and spent the morning in theatre with him. We had a delightful informal chat, I met some of the staff who I would eventually work with and I left feeling very optimistic. By this time I had just started my ST7 year and focus changed to ensuring I got all the experience and competencies I needed for my CCT. A nervous month or so passed by, Mr Watkin had had time to think about what he was letting himself in for and to my delight got in touch to tell me that in principle the job was mine. I still had to go through the formalities of application and interview but this happened much later. My advice to anyone thinking of applying to a competitive fellowship is to make contact early; currently recruitment to my fellowship will be for October 2019. The application process is quite similar to that of the consultant application form so this was a good introduction to future job applications.
The fellowship itself…
Most trainees in urology do not get exposure to a large volume of penile cancer and genitourethral reconstructive surgery. This was very evident when I first started. It was like being an ST3 on day one all over again. Of course, I knew the basics and had good surgical principles but the road ahead seemed very long. My initial offer was for a year, which I thought would be enough. I was wrong. From about month nine onwards I was getting in to the swing of things and I was fortunate to be given the chance to stay for another six months. This was definitely one of the best decisions I made. In the last six months I did a lot more independent operating and I felt more confident in my decision making, particularly in the benign cases about when to operate and when not to.
On top of the excellent clinical experience in St George’s and Epsom, I was able to take part in management roles, clinical research, teaching and also assisting in the private sector. My weekly timetable was protected from excessive service provision and this made a huge difference (Table 1).
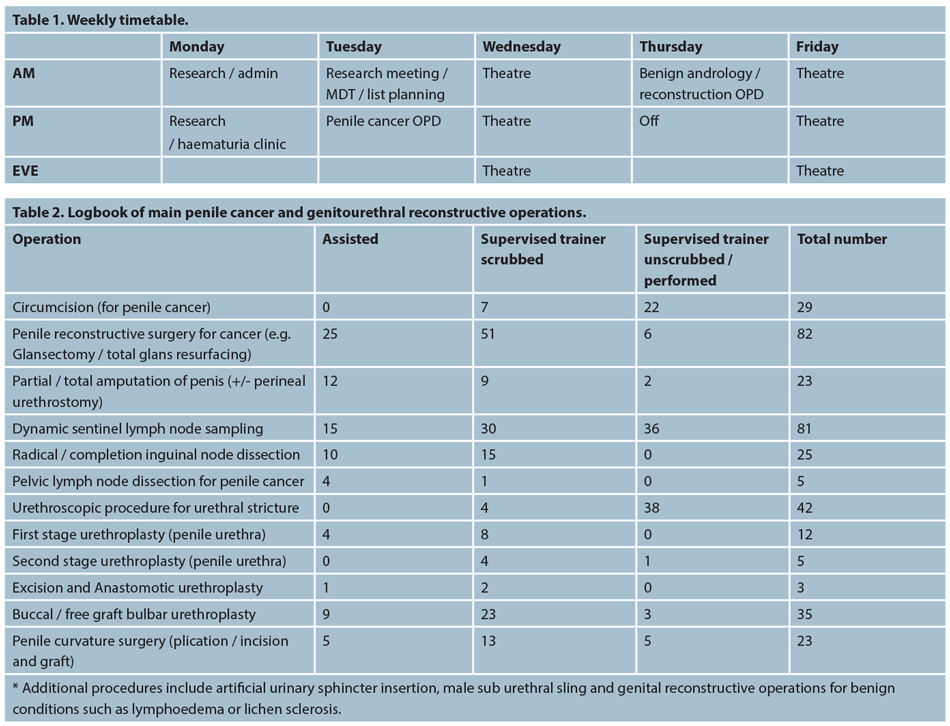
The operating was split mostly doing penile cancer on Wednesday and benign andrology / reconstruction on Friday. I took part in a one in eight middle grade on call rota. This allowed me to keep my hand in emergency and general urology given the very specialist nature of my normal week.
Penile cancer being a rare disease and urethroplasty also a relatively rare surgery means that the volume of cases seen cannot be compared to robotic or endourology fellowships for example. St George’s is the hub for a large penile cancer network and is one of the highest volume centres in Europe seeing around 100 new cases per year (Figure 1). I quickly transitioned from assisting to performing parts of each operation and ultimately performing some cases independently. This modular approach to training is common and works well for penile and urethral surgery (Table 2).

Figure 1. The award winning team at St George’s.
As I mentioned earlier there was so much more to this fellowship than penile and urethral surgery. I took part in medical student teaching, weekly departmental teaching, teaching at a urology higher surgical training training day and also giving a grand round lecture. I took on the responsibility of organising and running a benign andrology MDT every alternate week. I was the national trainee representative on the penile cancer subgroup at the National Cancer Research Institute (NCRI); this involved attending meetings / teleconference discussing the latest penile cancer research.
Research is an important part of the unit in St George’s. We had a weekly meeting lasting an hour or so discussing the ongoing projects and ideas for new projects. With Mr Watkin and the team’s assistance I was first author on three international abstracts presented at the SIU, EAU and AUA annual meetings, and one national presentation at BAUS. I had my name as second author on a further four international abstracts. In addition I had one oral presentation at a national meeting and had one paper published in a peer reviewed journal. One further paper has been submitted and two more getting ready for submission. For those without formal research experience this is a great opportunity to boost your CV with papers and presentations.
Was it worth it?
The simple answer is most definitely yes! My aim at the beginning of this fellowship was to develop the skills to manage penile cancer and urethral stricture disease to subspecialist consultant level. I think it would be naïve of me to think that I can do it all after an 18 month fellowship but I can certainly do a lot and I know what I can’t do and who to ask for help! As always there are too many people to thank but you can see many of the award winning team in the photo. The combination of high volume penile cancer and benign genitourethral reconstructive surgery is unique to any UK based fellowship and I would highly recommend this one to anyone who is interested.