In May/June 2016 we featured a wonderful account of Zeeshan Aslam’s first trip with Urolink to the Hawassa Referral Hospital in Ethiopia (see here). One year on we are delighted that Zeeshan has once again taken the time to provide us with a fantastic description of his second trip with the charity. We are sure many readers will be inspired to undertake their own professional adventures overseas.
In June 2015, after experiencing the most fascinating week of my professional life, I boarded my return flight from Addis Ababa airport back to London. I knew that I would be returning to Hawassa at some point, but I didn’t expect to be back on an Ethiopian Airlines plane again in less than six months, this time assigned to the BAUS Urolink transurethral resection of the prostate (TURP) workshop with Mr Graham Watson.

Graham with some of the street children of Ethiopia. Aberra starting TURP.
It was early in the morning on 3 December 2015 when I stepped outside the Addis Ababa airport; the feel of the cool morning breeze on my face brought back all the memories from my last visit. That sweet-scented smell was ever present in the air, the origin of which still remains unknown to me. Unsure if it is the fresh smell of plumeria or the metallic fragrance of burning eucalyptus leaves, I simply describe it as the gloriously intoxicating ‘scent of Ethiopia’.
Since childhood, my impression of Ethiopia has been of a country lacking the very basic necessities of life, with stretches of barren land and severe droughts and famines inflicted upon the population for generations. But now, this is a country known to me for its outstanding natural beauty and its kind people who boast a history rich in different cultures and religions. A country which can be proud of producing the world’s best long distance runners and probably the finest coffee I have ever tasted. This was a different Ethiopia for me now, the one I had witnessed, the one I was more familiar with.
”One of the challenges working in these conditions is the necessity of adapting to changing circumstances.”
The Hawassa urology resident Dr Getaneh Teferi was there to receive us and we were soon joined by Graham Watson who flew from Zimbabwe after finishing an exhausting percutaneous nephrolithotomy (PCNL) workshop in Bulawayo. Our goal for the trip was to focus on the two most common urological conditions encountered in Hawassa, benign prostatic hyperplasia (BPH) and urethral stricture disease. Since there is a lack of medical treatment for BPH due to financial constraints, the only treatment previously available to patients with lower urinary treatment symptoms (LUTS) and urinary retention was transvesical prostatectomy. The prime objective of Urolink workshops in Hawassa has been to provide training in performing TURPs to achieve an independent level of competency.

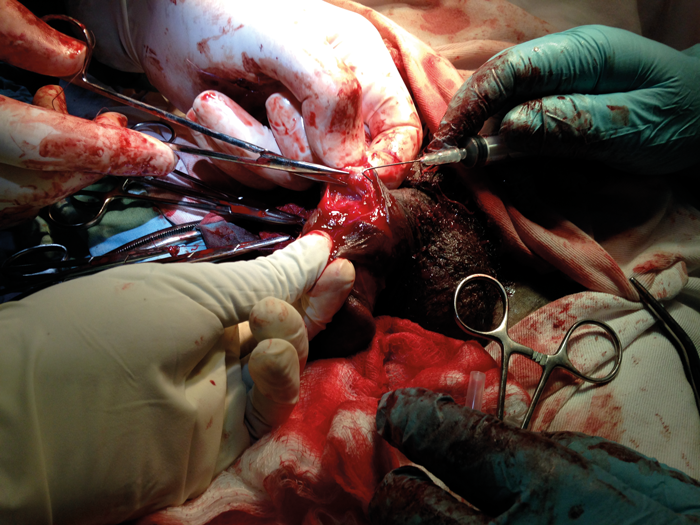
Aberra starting TURP.

Getaneh setting up for what was his first independent TURP.
We started our fascinating four-hour road journey from Addis Ababa to Hawassa and travelled through various villages. Those never-ending long muddy roads with scores of children standing on the sides waving at our jeep was a familiar scene, with their bare feet, dusty hair and torn clothes – but with the most precious bright faces and indescribably expressive smiles which seemed to belie all the troubles they face.
On our arrival in Hawassa, we visited the Referral Hospital to meet Consultant Urologist Dr Aberra Gobeze who was busy in the clinic. He briefed us about the cases he had listed for the week-long workshop. The endoscopy equipment kit, previously donated by Olympus, was in good functioning condition, ready to be used for the workshop. We had also taken with us other equipment such as resection loops, roller balls, bladder evacuators and guidewires. It was hugely encouraging to learn that a new theatre suite was under construction which, once completed, will provide more operating space and capacity.

Graham and Aberra discussing the new theatre plan.
Our routine was consistent with morning and postoperative ward rounds with a six-hour theatre session in between. On the first day, the workshop got off to a flying start with both Aberra and Getaneh performing TURPs, bladder neck incisions (BNI) and optical urethrotomy, demonstrating technique with clear improvement in their level of operative skill and overall confidence. Graham also demonstrated urethroplasty for penile stricture using a penile skin flap in a man who had been originally listed for an optical urethrotomy but was deemed unsuitable on the day. One of the challenges working in these conditions is the necessity of adapting to changing circumstances.
Our very innovative skin hook!
During urethroplasty there was a need for skin hooks, but as none were available, we created our own skin hooks by using a blunt 21 gauge needle bent at the tip and attached to a 10mls syringe. An innovative approach is essential for working in such circumstances.
The workshop continued for a week. The biggest problem we faced on this visit was frequent electricity cuts which, although for very short durations, occurred without any warning. This posed a big challenge while performing TURPs and we learnt the importance of meticulous haemostasis at all times during the procedure. We completed a total of 13 TURPs and one BNI. One patient failed to void postoperatively and one required blood transfusion. However, we were proud of the fact that Getaneh had become able to perform TURPs independently for the first time during the course of the workshop, and since then has continued to perform TURPs independently with good outcomes.

A typical Ethiopian forest house with its inhabitants.
During the week, Graham also discussed his plans of starting stone work at Hawassa with the host team. Both Getaneh and I benefitted from his teaching on PCNLs. We also spent time conducting assessments of the theatre staff on their knowledge of the assembly and care of urological endoscopic equipment, and teaching best practice.
Since my previous visit I had been very keen to visit the Ethiopian residents in the villages who make up the bulk of our patients, and to know more about the primary care set-up in Ethiopia. Over the weekend we went to visit the nearby village of Wondo Genet, where I witnessed a typical forest hut with its inhabitants. Though it was a fascinating experience, it reminded me of the great Australian obstetrician and humanitarian, Catherine Hamlin and her book The Hospital by the River where she describes obstetric fistula in remote parts of Ethiopia: “She may squat on the floor of her hut or lie in a thin straw mattress, sometimes for days on end, straining to deliver her baby. She is then, at last, able to expel her dead child.” It’s a sad reality that the process of childbirth in Africa causes an extremely high rate of vesico-vaginal fistulae (VVF).

Dedicated time of community health workers.
I was very impressed with the community medical centre that we visited in terms of the services provided and the cleanliness that was maintained there. There are about 30,000 such CMCs across Ethiopia. They conduct clinics for general medicine and TB, and perform minor procedures. One room in particular caught my attention, as it was a delivery room with a young woman in her 20s about to deliver her child. Whilst these CMCs no doubt do a remarkable job, my impression was that there remains a lot to be done for the promotion of good obstetric practice to reduce the very high incidence of VVF in Ethiopia.

Tuberculosis clinic at the CMC.
Once again the week passed in no time, but it felt truly satisfying as clearly both Graham and I had seen definite progress in Hawassa. We encouraged the host surgeons to continue performing TURPs on appropriately selected cases along with audit, teaching and ward rounds to maintain quality standards and governance. By the time of writing this article further work has been started in stone surgery and urethroplasties for stricture disease. Another positive that has happened for Hawassa Referral Hospital is that the urological trainee Getaneh has become a consultant now and is taking the department further, something which I hope to write about in the future.
After two visits so far to Ethiopia, I have come to the conclusion that the prime objectives of these workshops is no doubt the provision of services and infrastructural developmental work in low-income countries. But as a post-CCT urology trainee, I also benefitted significantly by gaining experience as a trainer in lower urinary tract endoscopic procedures especially while working in difficult circumstances. I would encourage senior urological trainees as well as consultants to get involved in these Urolink projects for both providing and gaining professional benefits.
Visit www.baus.org.uk/professionals/urolink/about/default.aspx for further information.

Acknowledgments
I am grateful to Urolink for entrusting me to conduct this workshop with Graham Watson. Once again, I would like to extend my gratitude to the host team for making arrangements for our visit and for their hospitality.
Please click here for Part 1 of this story.
Declaration of competing interests: None declared.




