There is no widely accepted system to classify postoperative complications. It is necessary to compare the outcome and complications while validating a new surgical procedure or one of the surgical approaches of a particular condition. Several parameters have long been used to determine the outcome of a procedure, including length of hospital stay, time to return to work, perioperative death, complication rates, and hospital costs, although no definitions for complications or guidelines for reporting surgical outcomes have been universally accepted.
Clavien-Dindo classification
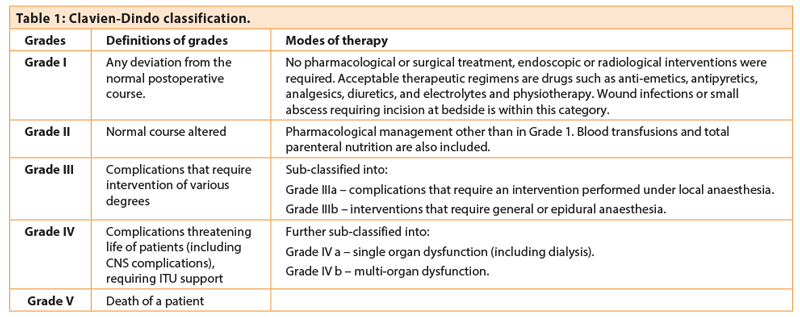
Clavien first introduced a classification of complications in 1992, based upon a cohort of 6336 patients who underwent elective hepato-biliary surgery [1]. To increase its applicability and reproducibility, Dindo modified Clavien’s original classification in 2004 by qualifying the type and mode of treatment applied to each complication [2]. As this modification is based upon objective data, it decreases the influence of subjective interpretation and prevents downgrading of the complications (Table 1).
Why do we need a uniform classification system?
The outcome of surgery is currently based on morbidity and mortality which can be measured by a process of audit. But an accurate and standard definition of surgical complications remains lacking in urologic surgery, which makes it difficult to measure morbidity. Although surgical complications are used to measure quality of surgery, the cause and effect relationship between surgery and complications is not always easy to establish. Furthermore, surgical complications vary with the surgeon’s skills, the learning curve for a new procedure and when the procedure had been performed. As an illustration, certain complications that were common in 2010 may not exist or be as common in 2015 as a consequence of the evolution of surgical knowledge regarding the disease process or the introduction of interventions for the prevention of those complications.
The use of a standardised, objective and easily reproducible classification system helps improve the quality of published scientific papers and allows health professionals, including medical authors, reviewers and editors, to evaluate the outcomes from a particular procedure. This will also help to analyse learning curves of surgical techniques as well as allowing better comparison between surgeons and institutions. A well accepted classification would allow urologists to accurately explain and compare different procedures to their patients in terms of risks and complications.
The European Association of Urology (EAU) strongly recommends the use of the validated Clavien-Dindo classification which has become widely used in the reporting of urological surgical outcomes, although until only a few years ago it was sparingly used in the literature. A current trend of increasing application of the Clavien-Dindo classification for categorisation of complications in urological surgery has been observed [3]. Descriptive forms of classification of postoperative complications were used in 62.7% of cases in 2010, whereas Clavien-Dindo was used in 33.3% of cases. The uptake of the Clavien-Dindo grade increased to 89.5% of cases in 2012 [3].
Disadvantages
The Clavien-Dindo classification is based upon the type of therapeutic intervention for complications occurring within 90 days of surgery. However, as interventions for the same complication may vary between institutions depending on the facilities available, there is inherent variability in the reporting of complications. Consequently there may be over-reporting and perhaps misplaced concerns regarding the reliability of a particular procedure when the type of anaesthesia and organ systems involved are considered in detail. For example, following percutaneous nephrolithotom (PCNL), bleeding can be managed by an interventional radiologist with angio-embolisation under local anaesthesia in one centre (Clavien-Dindo IIIa) or require general anaesthesia in another (Clavien-Dindo IIIb), leading to a discrepancy in grading the same complication. Similarly, another common clinical condition is the management of hydronephrosis secondary to obstruction, which may be managed by either insertion of a nephrostomy and ante-grade placement of a stent under local anaesthesia by an interventional radiologist (Clavien-Dindo IIIa) or by retrograde placement of a ureteric stent under general anaesthesia (Clavien-Dindo IIIb). This again leads to two different sub-categories of the same complication.
Another example is management of post-procedure colonic perforation which can be managed by early intervention under general anaesthesia by laparotomy (Clavien-Dindo IIIb) or alternatively it may be managed conservatively by intra-venous antibiotics and improved nutrition (Clavien-Dindo II).
The Clavien-Dindo classification also fails to distinguish between early and late postoperative complications; thus comparison of series with different follow-up periods may become questionable.
Use in different types of surgery for pelvic malignancy
Clavien-Dindo classification has already been validated in several retrospective case series as well as in randomised controlled trials to compare the grades of complications among open, laparoscopic and robot assisted surgery.
Cystectomy
An example of a classification of complications in post-cystectomy patients is given in Table 2.
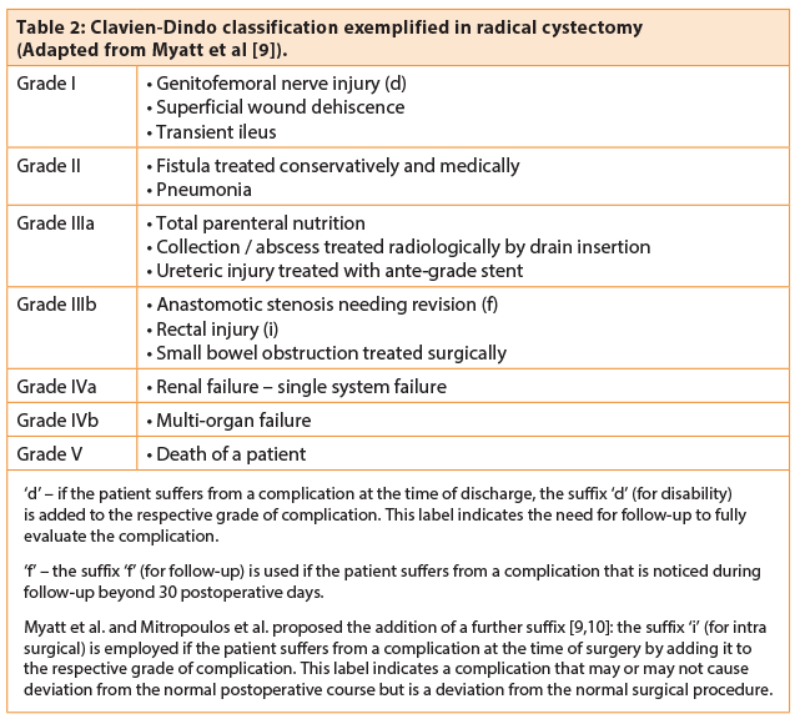
De Nunzio et al. performed a retrospective analysis of a cohort of patients in 19 centres in Italy over a period of one year [4]. They reviewed 467 patients with a mean age of 70 years who underwent radical cystectomy with urinary diversion. In 302 patients, they noted 415 complications which were classified as per Clavien-Dindo: 109 patients were Grade I; 220 patients grade II; 45 patients Grade IIIa; 22 patients Grade IIIb; 11 patients Grade IV; eight patients died (Grade V). Patients with cutaneous ureterostomy presented a lower rate (8%) of Clavien-Dindo Grade ≥IIIa. A longer operative time was an independent risk factor of Clavien-Dindo grade ≥III. The authors concluded that radical cystectomies were associated with a significant morbidity (65%) but a reduced mortality (1.7%) when compared to previous experiences.
Roghmann et al. performed a retrospective study of 535 patients with bladder cancer who had univariate and multivariable analyses for prediction of complications [5]. Covariates included were body mass index, Charlson Comorbidity Index, age, sex, American Society of Anaesthesiologists (ASA) Score, neoadjuvant chemotherapy, prior abdominal or pelvic surgery, localised tumour and urinary diversion type. Classification of postoperative complications within 90 days revealed that overall reported complications were 56.4% (Grade I-V); major complications 18.7% (Clavien-Dindo Grade III-IV); and mortality 3.9% (Grade V). The most common complications were Clavien-Dindo Grade I-II: namely infections (16.4%), bleeding (14.2%) and gastrointestinal complications (10.7%).
A systematic review by Ishii et al. compared robotic and open radical cystectomy for 748 patients over a period of 13 years [6]. Four hundred and sixty-one patients were in the robotic group and 287 patients in the open group. Clavien-Dindo III-IV complication grades in the open group were significantly higher. The mortality rate (Clavien V) was higher again in the open group (2.2%) compared with the robotic group (0.35%).
“The use of a standardised, objective and easily reproducible classification system helps improve the quality of published scientific papers and allows health professionals to evaluate the outcomes from a particular procedure.”
Prostatectomy
Various prostatectomy series have used the Clavien-Dindo classification system to classify their complications.
Hruza et al. performed a retrospective review of 2200 consecutive patients who underwent laparoscopic radical prostatectomy (LRP) between 1999 and 2008 in a single hospital [7]. LRP was performed using a transperitoneal (n=871) or extraperitoneal (n=1329) retrograde Heilbronn technique. Five surgeons operated on 96% of the patients. Minor complications occurred in 21.7% of patients (Clavien I: 6.8%; Clavien II: 14.9%); anaemia requiring transfusion (10.4%) dominated. Early re-interventions were necessary in 6.7% of patients (Clavien IIIa: 3.6%; Clavien IIIb: 1.5%; Clavien IV-a: 1.5%; Clavien IVb: 0.1%). Late Clavien IIIb complications occurred in 4.7% of patients – most of them were anastomotic strictures. Mortality was 0.1% (Clavien V). There was a significant decrease in overall complication rates over time, resulting predominantly from decreasing Clavien I–II events. Learning curves of third-generation surgeons plateaued earlier compared to the first generation (250 vs. 700 cases). No co-morbidities were included in their data, thus limiting this study.
Rabbani et al. compared the postoperative medical and surgical complications in a large series of 4592 patients between open (retropubic) and laparoscopic radical prostatectomy without preoperative hormones or radiotherapy [8]. After stratification, they found that 10.2% had medical complications and 20.1% were surgical. Classification into medical and surgical complications is a deviation from the original Clavien-Dindo classification system and has been used by various other authors as well. When looking at the medical complications within the 30 days postoperative period, 10% had Clavien-Dindo I-III, 1.7% had Grade III-V. On the other hand, 14.3% had Grade I-III, and 5.3% had Grade III-V surgical complications. Overall, in the open series, 8.8% and 18.7% had medical and surgical complications, whereas 14.5% and 24.5% had medical and surgical complications in the laparoscopic series, respectively. This distinction is useful for understanding the impact of comorbidity on surgical outcomes.
Conclusion
The Clavien-Dindo classification gives us an opportunity to record surgical complications in a standardised way and its routine use in all urology units is highly recommended. This would be in line with the increasing use of this system in the published literature and will enable us to compare our own outcomes with published data.
References
1. Clavien PA, Sanabria JR, Strasberg SM. Proposed Classification of Complications of Surgery with Examples of Utility in Cholecystectomy. Surgery 1992;111(5):518-26.
2. Dindo D, Demartines N, Clavien PA. Classification of Surgical Complications: A New Proposal with Evaluation in a Cohort of 6336 Patients and Results of a Survey. Annals of Surgery 2004;240(2):205-13.
3. Yoon PD, Chalasani V, Woo H. Use of Clavien-Dindo Classification in Reporting and Grading Complications after Urological Surgical Procedures: Analysis of 2010 to 2012. The Journal of Urology 2013;190(4):1271-4.
4. De Nunzio C, Cindolo L, Leonardo C, et al. Analysis of Radical Cystectomy and Urinary Diversion Complications with the Clavien Classification System in an Italian Real Life Cohort. European Journal of Surgical Oncology 2013;39(7):792-8.
5. Roghmann F, Trinh QD, Braun K. Standardized Assessment of Complications in a Contemporary Series of European Patients Undergoing Radical Cystectomy. International Journal of Urology 2014;21(2):143-9.
6. Ishii H, Rai BP, Stolzenburg J-U, et al. Robotic or Open Radical Cystectomy, Which Is Safer? A Systematic Review and Meta-Analysis of Comparative Studies. Journal of Endourology 2014;28(10):1215-23.
7. Hruza M, Weiss HO, Pini G, et al. Complications in 2200 Consecutive Laparoscopic Radical Prostatectomies: Standardised Evaluation and Analysis of Learning Curves. European Urology 2010;58(5):733-41.
8. Rabbani F, Yunis LH, Pinochet R, et al. Comprehensive Standardized Report of Complications of Retropubic and Laparoscopic Radical Prostatectomy. European Urology 2010;57(3):371-86.
9. Myatt A, Palit V, Burgess N, et al. The Uro-Clavien–Dindo system—Will the Limitations of the Clavien–Dindo System for Grading Complications of Urological Surgery Allow Modification of the Classification to Encourage National Adoption within the UK? British Journal of Medical and Surgical Urology 2012;5(2):54-60.
10. Mitropoulos D, Artibani W, Graefen M, et al. Reporting and Grading of Complications after Urologic Surgical Procedures: An Ad Hoc EAU Guidelines Panel Assessment and Recommendations. Actas Urologicas Españolas 2013;37(1):1-11.
Declaration of competing interests: None declared.
Part 2 of this feature can be found here.