A classification system of surgical complications was proposed by Clavien in 1992 [1] and further modified by Dindo in 2004 [2]. Clavien-Dindo classification has since then been validated through many retrospective case series as well as in comparative studies to standardise the complications and find out the superiority of one or other mode of treatment for a particular urological condition.
In our previous article we focused on the use of this classification system in urological pelvic cancer surgery. This article will address the use of this classification in upper tract surgery.
Nephrectomy
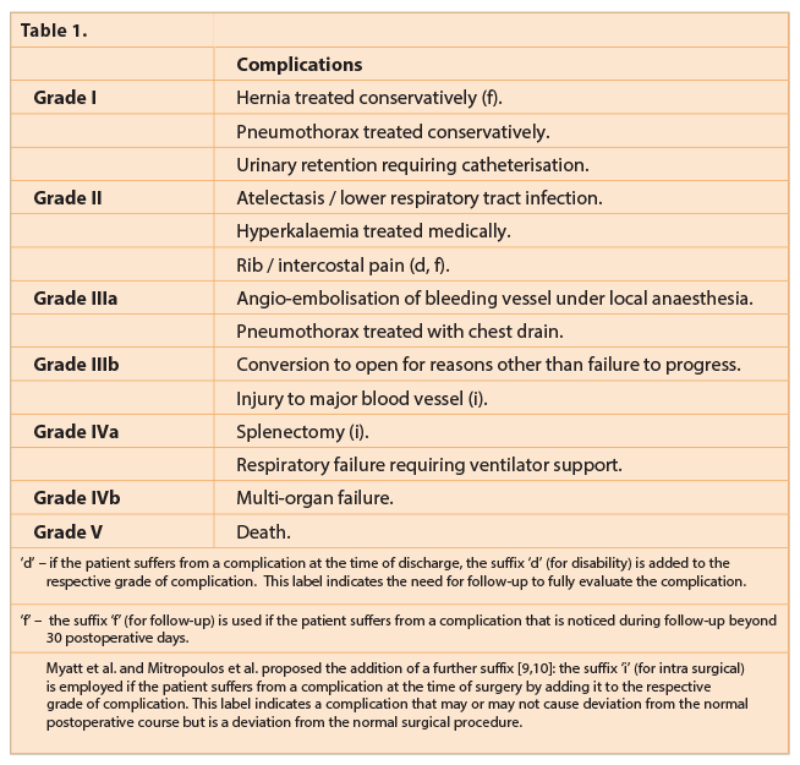
Various authors have applied the Clavien-Dindo system for describing complications post nephrectomy. In Table 1 we have listed some common complications classified according to the Clavien-Dindo system.
Hennus et al. performed a single-centre retrospective study of 198 patients with suspected renal cell carcinoma (RCC) undergoing open radical or partial nephrectomy, using modified Clavien-Dindo classification in terms of postoperative complications. The overall complication rate was 34%: grade I=7%, grade II=15%, grade III=5%, grade IV=3% and grade V=5%. Fifty-one percent of all patients had comorbidities. There were significantly more major complications in patients with major comorbidities at 16% vs. 7%. Patients with high-stage RCC had significantly more severe complications than low-stage RCC. The authors advised that the comorbidity scores can be used in risk stratification for complications and recommended to consider this during decision-making and counselling of patients before nephrectomy [3].
Khalifeh et al. performed a retrospective review of 427 patients who underwent transperitoneal robotic partial nephrectomy with or without hilar clamping with a follow-up of two to six years. Two intraoperative complications (1.5%) and five high-grade Clavien-Dindo complications (3.7%) occurred. The complications reported were: pleural injury – one, profuse bleeding – one, conversions: laparoscopic – four and open – one. A total of 25 postoperative complications were noted. The grade distribution was grade I=4, grade 2=16, grade IIIa=4, grade IIIb=1. There was a 20.2% upstaging of CKD postoperatively, but no patients required dialysis [4].
A retrospective comparative case series study of 189 patients with preoperative nephrometry scores was performed by Reifsnyder et al. Of these, 107 patients had laparoscopic partial nephrectomy whereas 82 underwent open partial nephrectomy. The open surgery group had higher nephrometry scores than the laparoscopic group (7.12.4 vs. 5.61.8). Operating time and hospital stay were shorter and estimated blood loss was lower in the laparoscopic group. At 30 days, more overall complications were noted in the open group, though more major complications were noted in the laparoscopic group. At 30 days, 19 and 22 patients in the laparoscopic and open groups respectively had developed complications of various grades (17.8% vs. 26.8%). Out of this, eight and three patients were grade III-V (7.5% vs. 3.7%). Whereas, at 90 days only two in each group (1.9% vs. 2.4%) had grade I-II complications. Higher body mass index and higher estimated blood loss were predictors of more overall complications. The complication rate in the laparoscopic group was similar to that in the open group [5].
Ramasamy et al. performed a retrospective review of 663 patients who underwent laparoscopic live donor nephrectomies and 101 laparo-endoscopic single site donor nephrectomies. They recorded their 30-day complication rate as per modified Clavien-Dindo classification. At 30 days there was no significant difference in the overall complication rate between the two groups (7.1% vs. 7.9%). There were eight major complications (grade III-V) in the laparoscopic living donor nephrectomy group but only one in the laparo-endoscopic single site group [6].
Ureteroscopy and laser lithotripsy for renal / ureteric stones
Modified Clavien-Dindo classification is a validated method that is being successfully used to grade complications encountered following endoscopic stone surgery. It has been found to be easy and not time-consuming. This classification can serve as a straightforward, standardised tool for comparisons, both within centres to facilitate auditing or among different centres.
A prospective study by Mandal et al. was one of the first to describe the complications of uretero-renoscopy (URS) using the modified Clavien-Dindo classification system. From August 2010 to November 2011, 120 patients (71 men and 49 women) underwent primary (previously un-stented) URS. Of the 120 patients, 36 (30%) experienced 79 complications. Clavien-Dindo complications encountered were as follows: grade I=38.3%, grade II=15%, grade IIIa=2.5%, grade IIIb=8.3%, grade IVA=0.8%, and grade IVb=0.8%. The incidence of complications was greater with stone size >10mm, mid versus distal ureteral location, impacted stones, and surgery performed by a junior trainee; it was not affected by the gender of patients, side of stone, or type of lithotripter used.
“Modified Clavien-Dindo classification is a validated method that is being successfully used to grade complications encountered following endoscopic stone surgery.”
Complications were associated with longer operative time (75 vs. 46.5 minutes), prolonged hospital stay (4.8 vs. 1.5 days), and decreased stone-free rate (64% vs. 97%). According to the authors the high rate of grade I complications seen in this study resulted from the prospective nature of this study, which documented even the minor, self-limiting but frequent complications, not recorded in earlier retrospective studies, such as transient haematuria, transient increase in serum creatinine, and elevated temperature [7].
The Clinical Research Office of the Endourological Society (CROES) study by de La Rosette et al., the largest series of patients (n=11,885) from 114 centres of 32 countries, showed a stone-free rate of 85.6% while using laser (in 49%) and pneumatic device (in 30.3%) principally on patients having stone in the kidney (n=1852), ureter (n=8676) and both (n=1145). Overall, postoperative complications were low (3.5%), the most frequent being fever (1.8%); bleeding requiring blood transfusion was in 0.2% of cases. Clavien-Dindo classification revealed: grade I=1.4%, grade II=1.3%, grade III=0.5%, grade IV=0.1% and grade V=0.04%. The majority of complications belonged to grade I and II [8].
Percutaneous nephrolithotomy (PCNL)
PCNL is indicated, as per European Association of Urology (EAU) guidelines, for large (generally more than 1cm in diameter), staghorn, multiple and complex lower pole stones. The EAU has recommended categorisation of postoperative complications using the Clavien-Dindo system. Complication rates for PCNL vary from 15-60%, but the Clavien-Dindo system has not been used in all studies. Variation of the complication rates is related to differing technical aspects of PCNL.
Akilov et al. retrospectively performed a case series of 1027 patients who had undergone prone PCNL (n=948) and ureteroscopy and laser lithotripsy (n=79). One hundred and eighty patients (17.5%) had 235 complications. Further breakdown of complications revealed one complication in 140 patients, two in 27 patients, three in 11 patients, and four in two patients. Secondary interventions were performed to rectify 59 complications: 33 of these without anaesthesia and 26 under general anaesthesia. Adapting Clavien-Dindo classification revealed: 64 grade I (6.2%), 111 grade II (10.8%), 33 grade IIIa (3.2%), 39 grade IIIb (3.8%), three grade IVa (0.3%), and none of grade IVb or V. Seventy percent of these complications were minor (i.e. grades I-II), and the remaining 30% were grade III-IV, as adjunctive invasive interventions and intensive care were required to treat them [9].
“Postoperative complications that may be deemed minor by a urologist may be considered differently by another specialist.”
Shin et al. retrospectively reviewed 698 cases of PCNL performed in a single centre. Of these, 236 patients had staghorn calculi (33.8%). Initial and overall stone-free rates were 69.9% and 88.8%, respectively. Two hundred and eighty-two patients developed 297 complications. Clavien-Dindo complication grades were reported as follows: grade I=12.6%, grade II=20.8%, grade IIIa=4.4%, grade IIIb=0.7%, grade IVa=0.9%, grade IVb=0.6%, and grade V=0.4%. Transient peri-nephrostomy catheter urine leakage (15.2%) was the most common complication, followed by transient fever >38 degree Celsius (11%) and transfusion (6.9%). Other individual complications occurred in less than 1.5% of cases. In patients with staghorn calculi, grade I, II, IIIb, and IVa complications were significantly more common, and all grade IVb and V complications occurred in patients with staghorn calculi only [10].
Seitz et al. performed a systematic review of the literature published from 2001 to 2011. Following PCNL in 7314 patients, no complications were reported in 76.7% of patients, whereas other graded complications were: grade I=11.4%, grade II=7.1%, grade IIIa=2.7%, grade IIIb=1.4%, grade IVa=0.4%, grade IVb=0.2% and grade V=0.04% [11].
Limitations of Clavien-Dindo classification in PCNL
In PCNL there are some limitations in classifying complications because some auxiliary treatment modalities (e.g. second-look PCNL, uretero-renoscopy, and extracorporeal shockwave lithotripsy) are part of routine stone management. Residual stones following PCNL are quite common. Depending upon the size of the residual stones, if further interventions are carried out, for example ESWL under procedural analgesic (grade IIIa), ureteroscopy and laser lithotripsy under general anaesthesia (grade IIIb), for a simple upper tract stone, then these are to be regarded as complications. But residual stones less than 3-4mm are possibly not complications as this is often the definition of a stone-free state and considered clinically insignificant by some. On the other hand, PCNL for a staghorn calculus is often followed by additional interventions which are more appropriately regarded as staged procedures rather than complications. A possible solution may be to modify the Clavien-Dindo classification system for PCNL in order to address these issues. Blood transfusion has been grouped under grade II. Bleeding with significant fall in haemoglobin that requires further intervention following PCNL should not be regarded as grade II but grade III instead, because the significance and severity of blood transfusion is no less than a change of nephrostomy performed under local anaesthesia, which is graded as IIIa [9].
Postoperative complications that may be deemed minor by a urologist may be considered differently by another specialist, leading to a different grading for the same complication. Infectious complications are frequently observed following PCNL. Transient postoperative pyrexia developed as part of systemic inflammatory response syndrome (SIRS), not requiring antibiotics, can be categorised as grade I, whereas sepsis with organ failure requiring intensive care is categorised as grade IV. On the other hand, patients with early signs of sepsis, without circulatory failure, requiring intensive antibiotic and fluid, should ideally be classified as grade III. Radiological support is an inherent part of post-PCNL care, which is not a component of this classification. It has been shown that CT detects more post-PCNL complications than other diagnostic radiological tools. Therefore, use of plain X-Ray KUB to detect residual stone would lead to undiagnosed complications and under-grading of complications in this classification system. In other words, higher detection of complications and consequent secondary interventions would have led to higher grades of complications as per the Clavien-Dindo classification. This classification also does not incorporate patients’ comorbidities that may contribute to post operative complications.
Conclusion
The use of Clavien-Dindo classification has increased over the last few years in many areas of urological surgery, although it has not yet been universally accepted. Its widespread use will improve the care of urological patients by enabling the use of a standardised reporting system for outcomes. It is therefore highly recommended to continue to use it to classify postoperative complications in all urological surgery, in spite of its recognised limitations.
References
1. Clavien PA, Sanabria JR, Strasberg SM. Proposed classification of complications of surgery with examples of utility in cholecystectomy. Surgery 1992;111(5):518-26.
2. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Annals of Surgery 2004;240(2):205-13.
3. Hennus PML, Kroeze SGC, Bosch JLHR, Jans JJM. Impact of comorbidity on complications after nephrectomy: use of the Clavien classification of surgical complications. BJU International 2012;110(5):682-7.
4. Khalifeh A, Autorino R, Eyraud R, et al. Three-year oncologic and renal functional outcomes after robot-assisted partial nephrectomy. European Urology 2013;64(5):744-50.
5. Reifsnyder JE, Ramasamy R, Ng CK, et al. Laparoscopic and open partial nephrectomy: complication comparison using the Clavien system. Journal of the Society of Laparoendoscopic Surgeons 2012;16(1):38-44.
6. Ramasamy R, Afaneh C, Katz M, et al. Comparison of complications of laparoscopic versus laparoendoscopic single site donor nephrectomy using the modified Clavien grading system. The Journal of Urology 2011;186(4):1386-90.
7. Mandal S, Goel A, Singh MK, et al. Clavien classification of semirigid ureteroscopy complications: a prospective study. Urology 2012;80(5):995-1001.
8. De la Rosette, J, Denstedt J, Geavlete P, et al. The clinical research office of the endourological society ureteroscopy global study: indications, complications, and outcomes in 11,885 patients. Journal of Endourology 2014;28(2):131-9.
9. Akilov FA, Giyasov SI, Mukhtarov ST, et al. Applicability of the Clavien-Dindo grading system for assessing the postoperative complications of endoscopic surgery for nephrolithiasis: a critical review. Turkish Journal of Urology 2013;39(3):153-60.
10. Shin TS, Cho HJ, Hong SH, et al. Complications of percutaneous nephrolithotomy classified by the modified Clavien grading system: a single center’s experience over 16 years. Korean Journal of Urology 2011;52(11):769-75.
11. Seitz C, Desai M, Häcker A, et al. Incidence, prevention, and management of complications following percutaneous nephrolitholapaxy. European Urology 2012;61(1):46-58.
12. Myatt A, Palit V, Burgess N, et al. The Uro-Clavien–Dindo system—will the limitations of the clavien–dindo system for grading complications of urological surgery allow modification of the classification to encourage national adoption within the UK? British Journal of Medical and Surgical Urology 2012;5(2):54-60.
13. Mitropoulos D, Artibani W, Graefen M, et al. Reporting and grading of complications after urologic surgical procedures: an ad hoc EAU guidelines panel assessment and recommendations. Actas Urologicas Españolas 2013;37(1):1-11.
Declaration of competing interests: None declared.





