Case 1
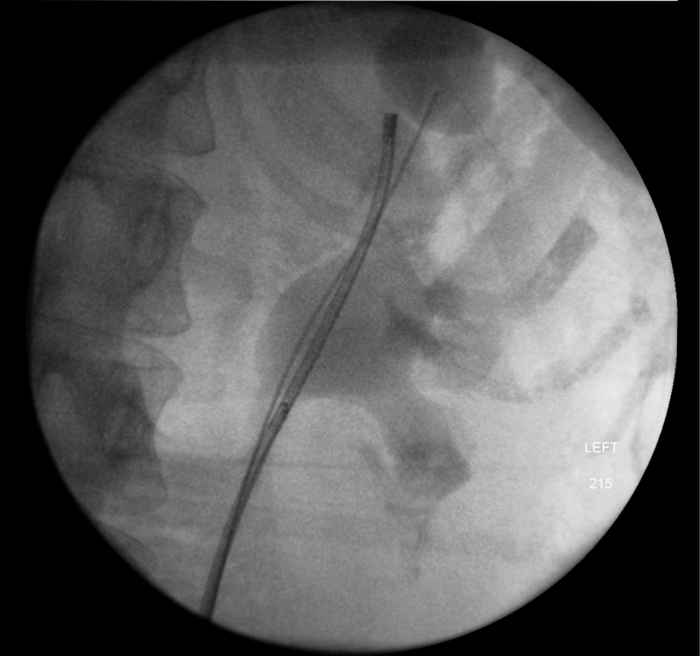
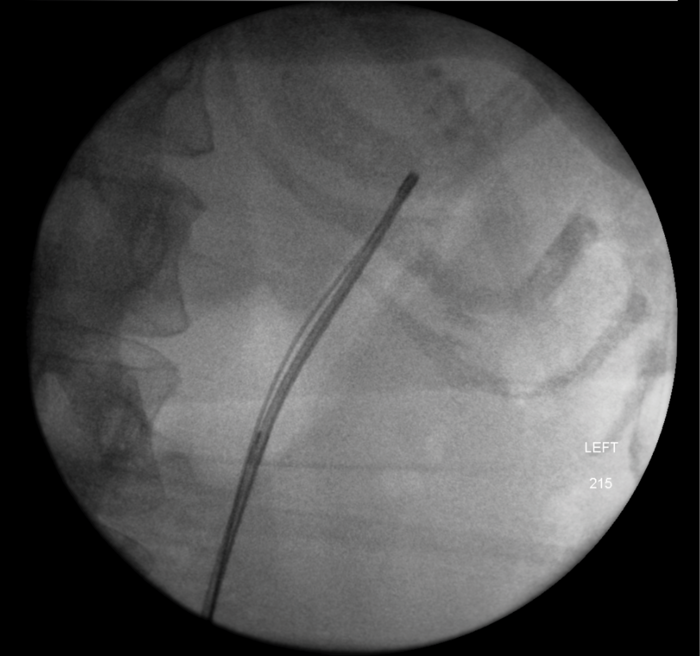
A 78-year-old male was transferred from a referring hospital. He had a cystectomy and ileal conduit performed 15 years previously and had recently been admitted with a clinical diagnosis of an infected obstructed kidney. The referring hospital had sited bilateral antegrade ureteric stents and were unable to remove the stent on the left side when the sepsis had settled. He had a long tortuous ileal conduit which was difficult to endoscope. A safety guidewire was placed retrogradely into the left kidney and after considerable manipulation, the stent was removed but the wire displaced and could not be replaced. Interestingly, some of the strings were still attached to the proximal end of the stent which may have led to difficulty with extraction. A perioperative loopogram demonstrated free reflux up both sides and the patient made an uncomplicated recovery, stent free.

Figure 1: Perioperative loopogram. Red arrow – Foley catheter in long tortuous conduit. Green Arrow – reflux into right upper tract.
Learning points
-
Upper tract dilatation is of course normal after an ileal conduit and stents may not have been necessary to manage this patient’s upper tract infection.
-
Strings need removing from antegrade ureteric stents.
-
Stent changes into ileal conduits can be very difficult and the stent can dislodge. The conduitoscopy can be challenging.
Case 2
A 44-year-old woman presented with left flank pain and stones in an upper pole diverticulum. She had undergone a failed percutaneous nephrolithotomy (PCNL) and flexible ureteroscopy in another hospital.

Flexible ureteroscopy and a retrograde pyelogram demonstrated the upper pole calyceal diverticulum with a pinpoint infundibulum entrance. The entrance was opened using a holmium laser on a low power setting and the stones dusted to allow spontaneous passage. A stent was placed into the diverticulum and left for four weeks. The patient was subsequently stone free.
Learning points
-
PCNL into a calyceal diverticulum with no apparent exit is technically demanding.
-
Flooding the collecting system with dilute methylene blue followed by drainage can delineate a difficult to locate infundibulum (find the blue dot).
-
Holmium laser infundibulotomy is a useful technique but be prepared for haemorrhage and include this outcome during informed consent. If significant bleeding is encountered and cannot be controlled, a stent and angiography are possible outcomes. Place a three way irrigating bladder catheter at the end of the case.
Case 3
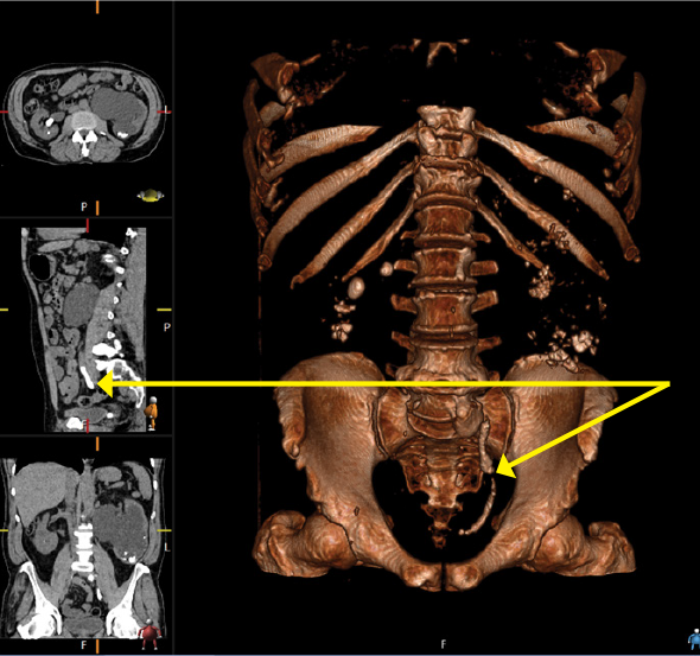
An 80-year-old woman presented with urosepsis requiring direct admission to intensive care. A CT scan demonstrated gas in the collecting system and a nephrostomy was inserted.


Figure 1: CT demonstrating gas in the collecting system.

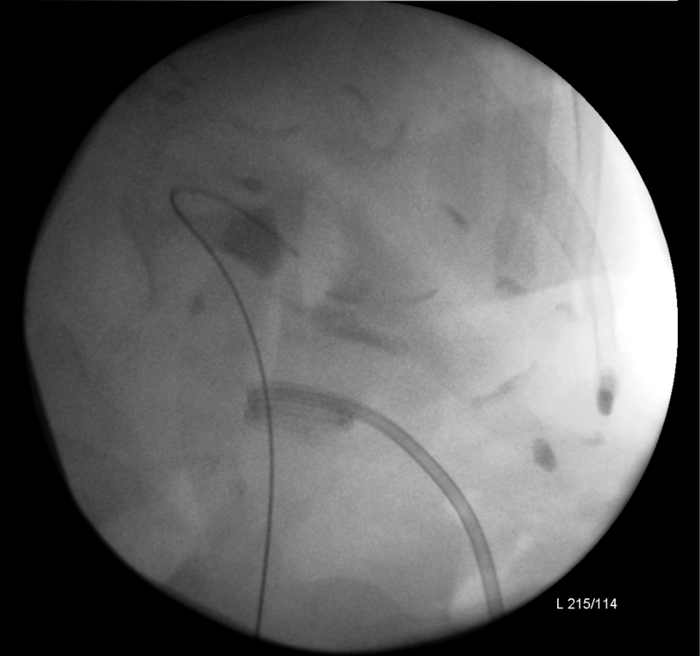
Figure 2: Nephrostogram showing stone in left kidney with nephrostomy in place prior to flexible ureteroscopy.
The patient made a good recovery from her life-threatening sepsis, retaining function on a DMSA scan and underwent a flexible ureteroscopy to clear the stone. Gas forming organisms in the urinary tract result in dramatic imaging but should not distract from the patient’s clinical condition. A conservative approach may avoid a nightmare nephrectomy in a highly morbid patient.
Learning points
-
Gas forming infection in the collecting system is a dramatic finding on imaging. Management may not need to differ from non-gas forming urinary tract infection.
Case 4
A 57-year-old male presented with right flank pain. He had an established diagnosis of medullary sponge kidney and had been lost to follow-up. Serum creatinine was 114.
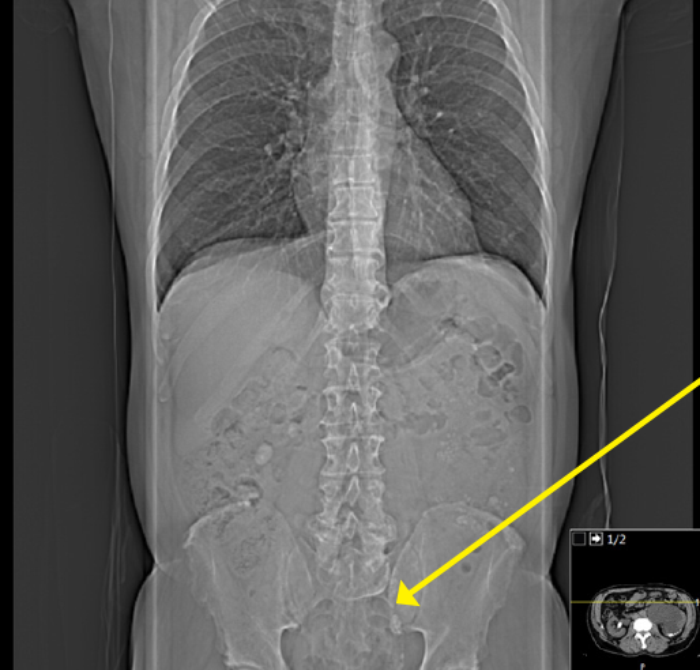
Figure 1: CT scout film demonstrating left ureteric stone on the opposite side to the patient’s pain.
Figure 2: 3D CT reconstruction demonstrating stone burden.
Learning points
-
This is an example of a rarely seen ureteric stone burden.
-
Questions - What is the split renal function?
- Is this kidney worth salvaging?
- Is the patient fit for intervention?
- In an asymptomatic, frail elderly patient, is no treatment an option?