Treatment of prostate cancer in renal transplant recipients is challenging due to a lack of knowledge of the natural history of cancer in these patients, the anatomical position of the graft in the iliac fossa and its proximity to the surgical or radiation field, and the ongoing immunosuppressive state of these patients.
We present a case of a renal transplant recipient due to hypertensive nephropathy. He was later diagnosed with intermediate unfavourable risk prostate cancer.
Case report
A 55-year-old male had chronic renal failure requiring initial peritoneal dialysis. He had a renal transplant from his partner four years ago. His initial prostate specific antigen (PSA) during the transplant work-up was one. This increased to nine within two years. Another increase in PSA triggered an MRI scan of the prostate which revealed a PI-RADS 5 lesion, T3a in a 20cc prostate. He proceeded to a transperineal prostate biopsy which revealed a Gleason 4+3 cancer with a maximum cancer length of 10mm. Staging prostate specific membrane antigen positron emission tomography (PSMA PET) scan showed no nodal or distant metastasis. He is on regular tacrolimus, anti-hypertensive and insulin. He has a functioning renal transplant.
Overall, this is localised prostate cancer with intermediate unfavourable risk. His recommended option is active treatment such as focal therapy, radical prostatectomy or radical radiotherapy with androgen deprivation therapy.
He proceeded to a robotic radical prostatectomy. It was uncomplicated with a few technique modifications discussed below. Final histology showed Gleason score 4+3=7 with a clear margin. Pathological stage pT3b.
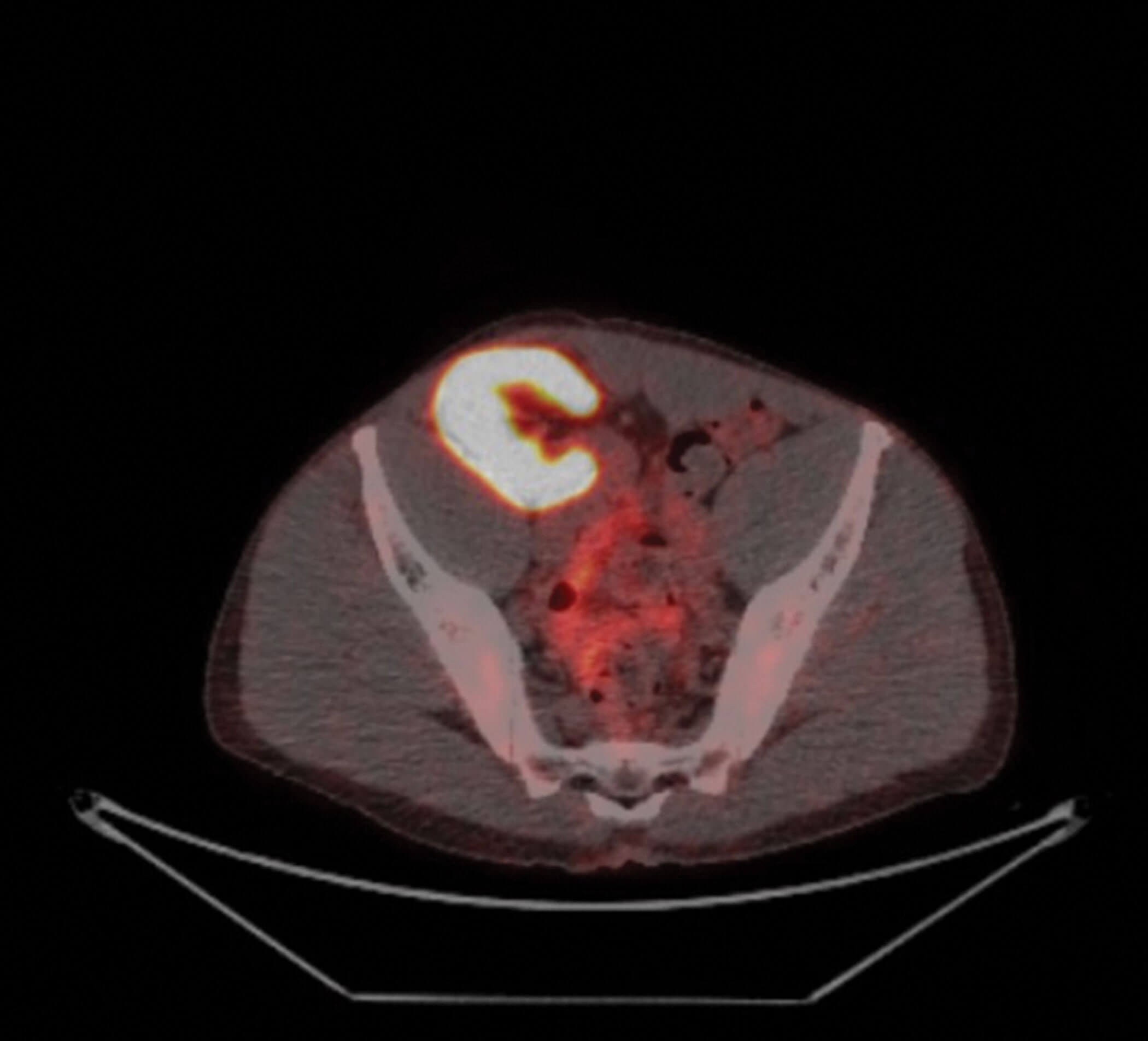
Figure 1: Renal transplant at the level of the iliac crest.
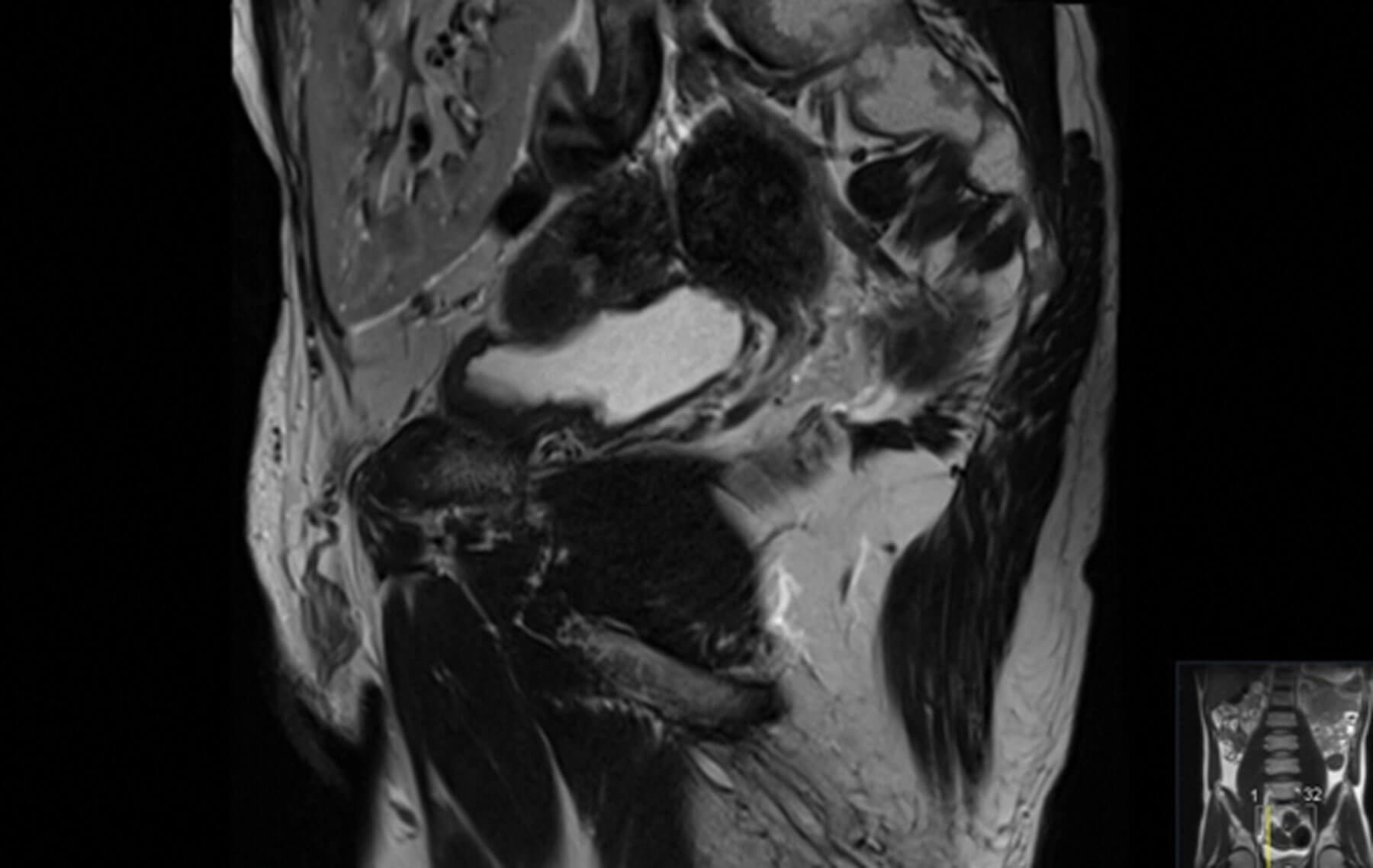
Figure 2: Sagittal image of MRI prostate showing
the proximity of renal transplant to the bladder.
Discussion
Natural history of prostate cancer in renal transplant recipients
The benefit of prostate cancer screening in the general population is a matter of controversy. The Kidney Disease Improving Global Outcomes (KDIGO) clinical practice guidelines state, “No advice is given for or against screening for prostate cancer” in kidney transplant recipients “beyond following local recommendations / standards for prostate cancer screening in the general population.”
In the current era of renal transplant and the expansion of eligibility criteria to older recipients, there are growing concerns about prostate cancer detection and treatment in these patients.
There are also concerns regarding anti-rejection drugs and their links to malignancy. Calcineurin inhibitors such as tacrolimus have been associated with enhanced in vitro and in vivo prostate cancer aggressiveness. Some research noted that genitourinary malignancies occur at a higher incidence in the transplant population compared to the general population, but the incidence of prostate cancer is not increased. There are also other unique risk factors for post-transplant malignancy including exposure to oncogenic viruses and underlying medical conditions which are common in patients with renal failure.
In short, there is a lack of knowledge of the cancer natural history hence while some suggest increased incidence of prostate cancer in renal transplant recipients, some suggest otherwise [1].
In our centre, PSA screening is done before renal transplantation. This screening is done using PSA testing and a digital rectal examination, similar to the screening done in the general population.
Radical prostatectomy in renal transplant recipient
A systemic review has demonstrated that the majority of renal transplant recipient patients with localised prostate cancer were treated with radical prostatectomy (82%) compared to external beam radiotherapy (12%) or brachytherapy (6%) [2].
Any treatment for prostate cancer in renal transplant recipients poses a few difficulties. Firstly, we have to avoid direct or indirect injury to the anatomical location of the transplanted kidney which may occur from surgery or from radiation. We have to also consider the effect of peritoneal dialysis or adhesions and the potential need for further transplants in case of graft failure.
There are many described modifications for performing robotic radical prostatectomy in renal transplant recipients including medial movement of trocars placement, assistant port on the contralateral side of the renal transplant, exclusion of the port closest to the transplant, the use of Retzius sparing technique or consideration of extraperitoneal approach.
In our centre, the open Hasson technique is used to place the initial camera port cranial to the umbilicus in the midline. The patient is then placed in a steep Trendelenburg position. Once the pneumoperitoneum is established, the remaining 8mm robotic trocars are placed. Our assistant port on the right side, which is usually the ipsilateral side of the renal transplant, is shifted cranially a few centimetres and inserted under direct vision. In this case, we also inserted a 10mm assistant port in the upper quadrant instead of the usual 5mm port to enable clips to be applied from both ports.
Overall, the surgical approach should be guided by the surgeon’s experience. The presence of the renal transplant requires careful placement of the trocar, especially the lateral ports and awareness when retracting / assisting and pressure on the kidney and the transplant ureter.
Of the 47 patients in the systemic review [1], one required a conversion to open because of exposure difficulties and two rectal injuries were reported. There were also three ureteric injuries with two recognised and fixed intraoperatively, and one subsequent ureteric stricture.
A recent study suggested preoperative planning with an excretory CT scan to visualise the ureter location [2]. We did not perform this scan but had a routine planning meeting preoperatively with an experienced radiologist to run through the MRI for anatomical consideration and appropriate nerve-sparing cases. Preoperative stenting can be considered to assist in identification of the ureter.
In our series of 16 men from 2010 to 2017, our mean blood loss was 323ml and mean operating time was 191 minutes. We had one partial ureteric injury which was repaired intraoperatively. Fourteen out of the 16 men had undetectable PSA at a median follow-up of 15 months.
Oncological outcomes
In a systemic review, the cancer specific and overall survival rates were 92.4% and 92.4%, respectively. These medium-term follow-ups were similar to those with non-renal transplant series [1]. Of the five deaths, four were prostate cancer and / or graft-unrelated while one patient had persistently elevated postoperative PSA levels and developed metastatic castrate resistant prostate cancer five months later.
Functional outcome
Continence rates were reported as ranging from 65% to 100% whereas potency rates ranged from 25% to 100% [1].
Another treatment option for prostate cancer is radiotherapy. Some experts consider renal transplantation as a contraindication to prostate radiotherapy. On the other hand, brachytherapy is considered less harmful. As kidneys are radio-sensitive, there are many concerns with regard to radiation nephritis and ureteric anastomotic stricture. A recent review showed that toxicity and complication rates were acceptable and no therapy-related graft loss was recorded.
Overall, radical prostatectomy in renal transplant recipients has a high rate of success and has an acceptable complication rate. This is still the preferred approach.
Conclusion
The evidence is scant in addressing prostate cancer for renal transplant recipients. We have described our thought process and evidence gathering as well as sharing our centre’s experience in performing robotic radical prostatectomy in renal transplant recipients.
References
1. Marra G, Dalmasso E, Agnello M, et al. Prostate cancer treatment in renal transplant recipients: a systematic review. BJU Int 2018;121(3):327-44.
2. Hevia V, Boissier R, Rodríguez-Faba Ó, et al. Management of localised prostate cancer in kidney transplant patients: a systematic review from the EAU Guidelines on Renal Transplantation Panel. Eur Urol Focus 2018;4(2):153-62.
3. Marra G, Agnello M, Giordano A, et al. Robotic radical prostatectomy for prostate cancer in renal transplant recipients: results from a multicenter series. Eur Urol 2022 [Epub ahead of print].