Case 1
A 67-year-old gentleman underwent a CT scan after presenting with visible haematuria and weight loss. His comorbidities include hypertension, type II diabetes mellitis and hypercholesterolaemia. He is a smoker.
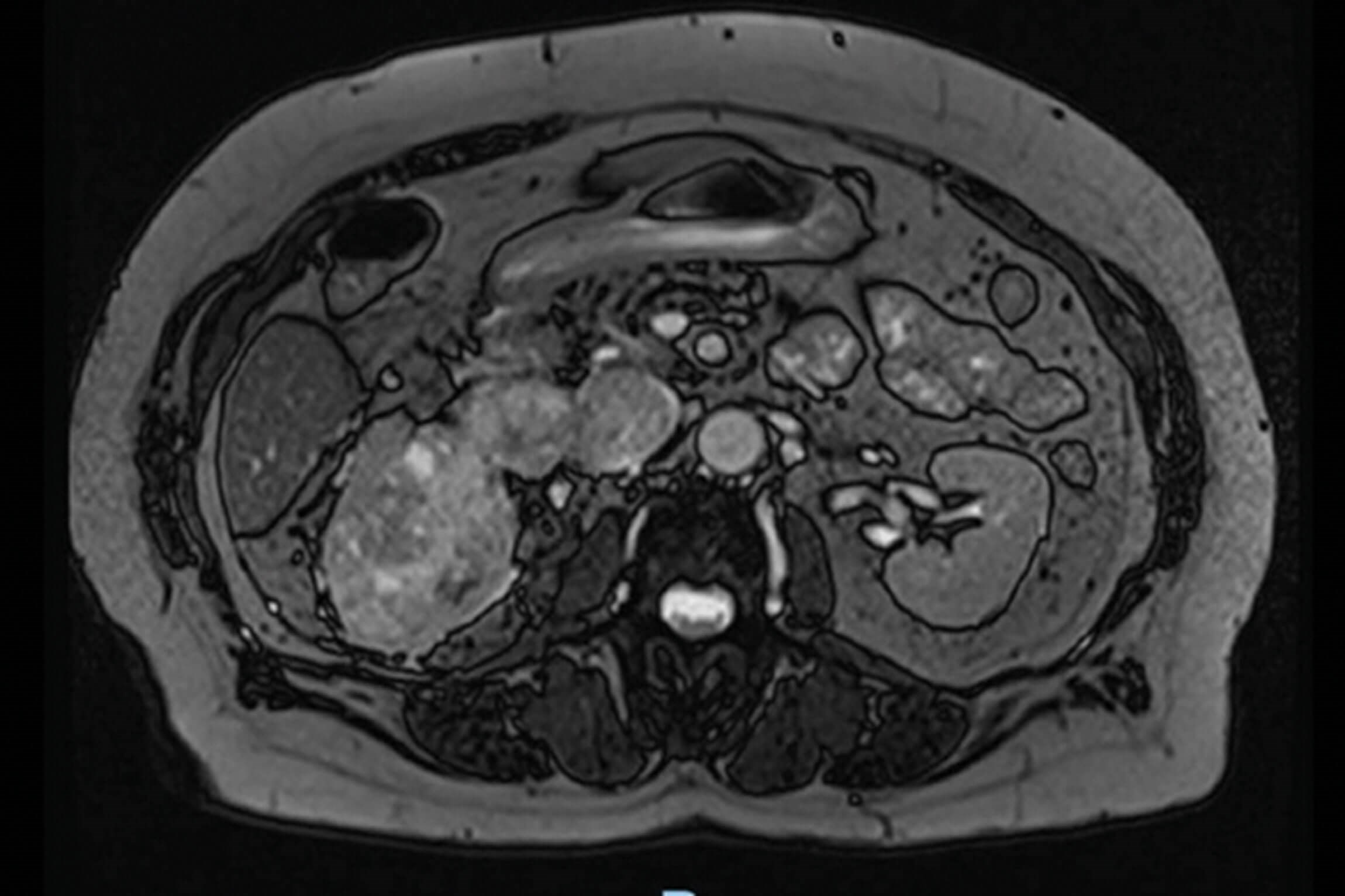
Figure 1.
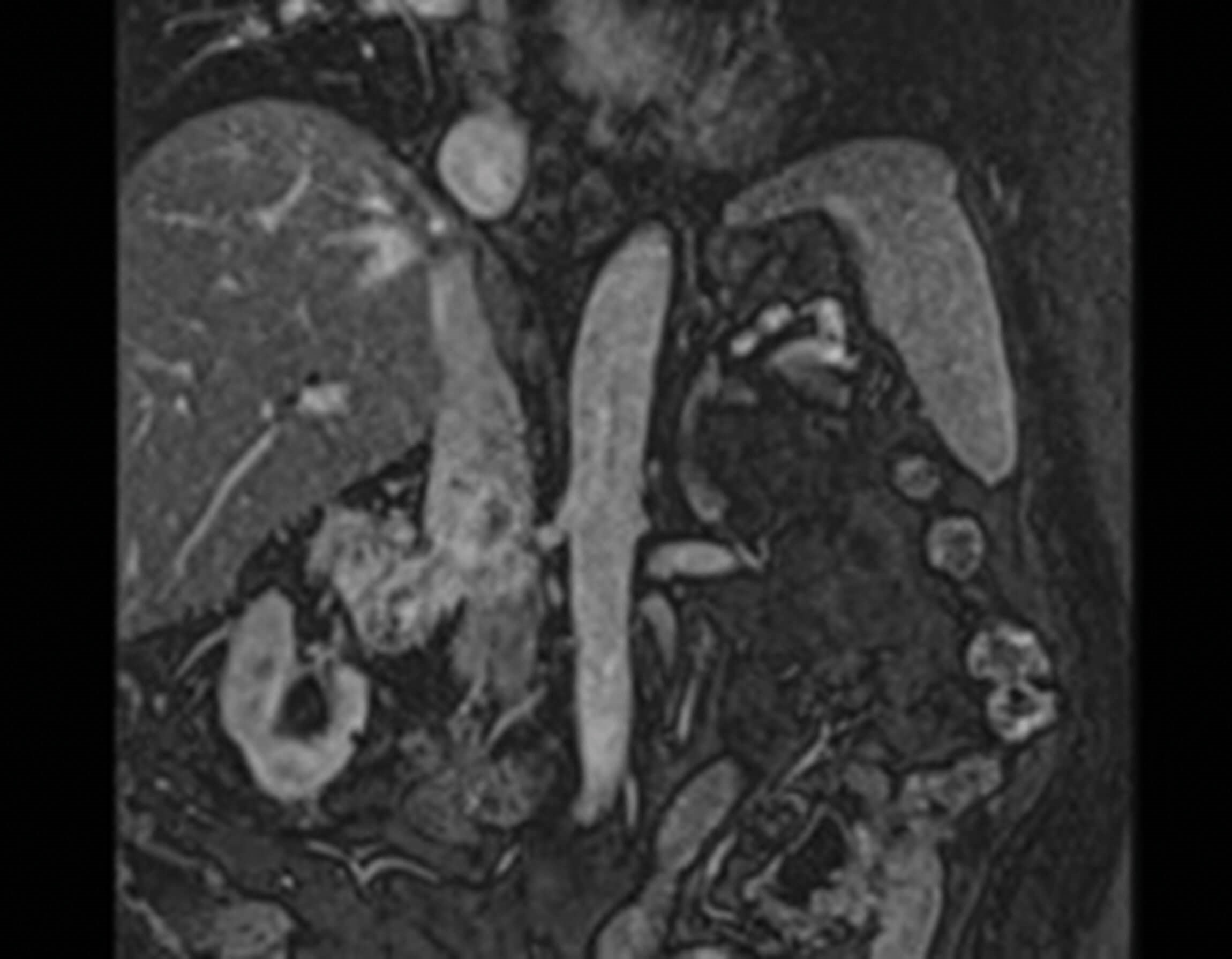
Figure 2.
- What do Figures 1 and 2 demonstrate? What is the stage of this lesion?
- What are this patient’s management options?
- What is the prognosis associated with these lesions?
Case 2
A 78-year-old gentleman underwent a CT for weight loss, shortness of breath and iron deficiency anaemia. He has a previous history of cerebrovascular accident for which he takes aspirin and has chronic kidney disease.

Figure 3.
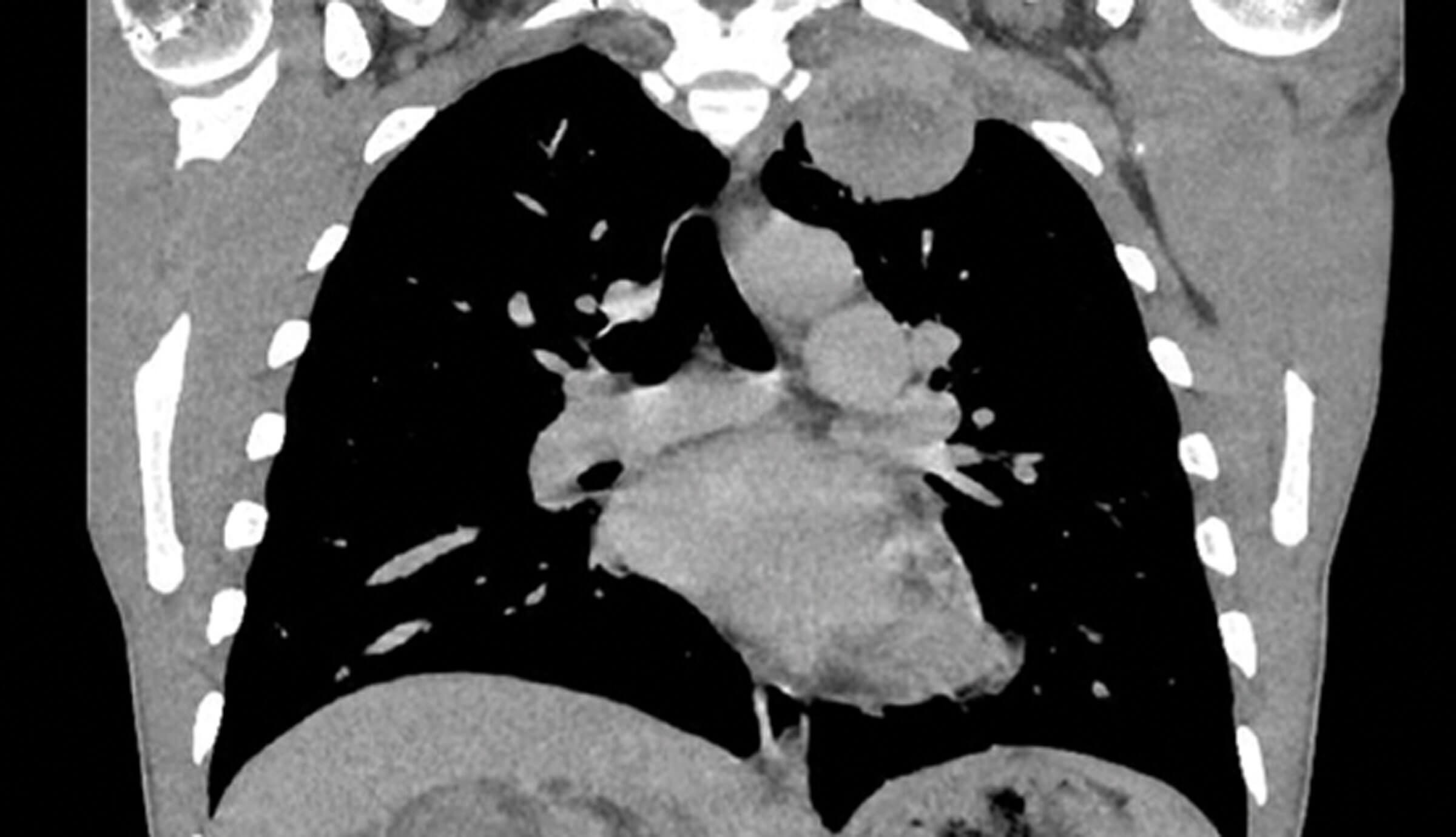
Figure 4.
- What do Figures 3 and 4 demonstrate?
- What a re the management options for this case?
- What’s the role of cytoreductive nephrectomy in these cases?
Answers
Case 1
1. This is an axial and coronal section of an MRI, which demonstrates a large right renal tumour. The tumour extends into the inferior vena cava but remains below the diaphragm. This patient therefore has T3bN0Mx disease. RCC staging follows the TNM staging outlined in article 1 ‘Localised Renal Cancer’.
2. T3b renal cancers may be managed with an aggressive surgical approach if the patient is surgically fit and wishes to opt for this [1]. Typical management options include:
- Radical nephrectomy with inferior vena cava (IVC) thrombectomy: Removal of the affected kidney along with the IVC tumour thrombus, is a complex and challenging procedure often performed via an open, and more recently robot-assisted, approach which requires vascular surgery input. Intraoperative techniques such as circulatory bypass may be employed based on the extent of the thrombus.
- Neoadjuvant / systemic therapy: In selected patients with extensive thrombus or borderline resectable disease, neoadjuvant targeted or immunotherapy may be considered to downsize the tumour and thrombus, potentially facilitating a subsequent complete resection. However, the evidence is still evolving, and its use remains on a case-by-case basis.
- Adjuvant therapy: Postoperative systemic therapies may be considered in high-risk cases or if adverse pathological features are present (e.g. positive margins), although the benefit of adjuvant treatment in T3b renal cell carcinoma (RCC) continues to be investigated. For patients unfit for major surgery, palliative systemic therapy might be the only option, although these are associated with poorer prognoses.
3. Five-year survival rates for T3b tumours are estimated to be 40–60%, though outcomes can vary widely. Prognosis is influenced by factors such as tumour grade, extent of venous involvement, surgical resection margins, and overall patient health. While aggressive surgical management can improve outcomes in carefully selected patients, there remains a significant risk for local recurrence and distant metastasis. Consequently, a multidisciplinary approach and consideration of adjuvant systemic therapies is critical in optimising long-term survival.
Case 2
1. Figure 3 is a coronal section of an arterial phase CT and demonstrates a large, heterogenous, solid, right tumour, which extends beyond Gerota’s fascia. Figure 4 is a coronal section of a thoracic CT demonstrating a left superior thoracic metastasis. These images demonstrate RCC with thoracic metastasis.
2. The mainstay of treatment is systemic therapy. All treatment options are outlined below [1]:
- Systemic therapy: Targeted therapy agents such as tyrosine kinase inhibitors, or TKIs (e.g. sunitinib, pazopanib, cabozantinib) help inhibit angiogenesis and tumour growth. Immune checkpoint inhibitors (e.g. nivolumab) a programmed death inhibitor (PD-1), have shown improved survival [2]. Initial results for targeted therapy (e.g. tyrosine kinase inhibitor) with immunotherapy appear promising [3].
- Surgical interventions: In patients with good performance status and limited metastatic burden, cytoreductive nephrectomy (removal of the primary tumour) combined with systemic therapy may improve outcomes. However, one large study found patients with an estimated survival of <12 months and ≥4 poor prognostic indicators would not benefit from this [4]. For patients with oligometastatic disease, resection of metastatic lesions can be considered, potentially prolonging survival. Complete removal of metastases have proven to be effective [5].
- Palliative care: Symptom management and supportive care are crucial, particularly for patients with extensive metastatic disease or poor functional status.
3. Cytoreductive nephrectomy is both relatively novel and controversial. The primary aim is to reduce tumour burden, theoretically enhancing subsequent systemic treatment efficacy (such as targeted therapies and immunotherapies). This approach is considered in patients with good performance status and limited metastatic burden. A meta-analysis of 56 studies concluded that receiving systemic therapy is the priority in patients with metastatic RCC [6]. Moreover, cytoreductive nephrectomy should be reserved for those who responded well to systemic therapy and with positive prognostic factors [7].
References
1. Ljungberg B, Bensalah K, Canfield S, et al. EAU guidelines on renal cell carcinoma: 2015 update. Eur Urol 2015;67(5):913–24.
2. Jain RK, Sarfraz H, Farooq MZ, Sonpavde G. ‘Management of metastatic renal cell carcinoma’. In: Singh P, Nayak B, Panaiyadiyan S (Eds.). A Guide to Management of Urological Cancers. Springer; Singapore; 2023.
https://doi.org/10.1007/978-981-99-2341-0_4
[Link last accessed October 2025].
3. Peinemann F, Unverzagt S, Hadjinicolaou AV, Moldenhauer I. Immunotherapy for metastatic renal cell carcinoma: a systematic review. J Evid Based Med 2019;12(4):253–62.
4. Garje R, An J, Greco A, et al. The future of immunotherapy-based combination therapy in metastatic renal cell carcinoma. Cancers 2020;12(1):143.
5. Heng DYC, Wells JC, Rini BI, et al. Cytoreductive nephrectomy in patients with synchronous metastases from renal cell carcinoma: results from the international metastatic renal cell carcinoma database consortium. Eur Urol 2014;66(4):704–10.
6. Zaid HB, Parker WP, Safdar NS, et al. Outcomes following complete surgical metastasectomy for patients with metastatic renal cell carcinoma: a systematic review and meta-analysis. J Urol 2017;197(1):44–9.
7. Bhindi B, Abel EJ, Albiges L, et al. Systematic review of the role of cytoreductive nephrectomy in the targeted therapy era and beyond: an individualized approach to metastatic renal cell carcinoma. Eur Urol 2019;75(1):111–28.







