Case 1
A 56-year-old lady is referred to the urology clinic after the GP conducted an ultrasound abdomen for deranged liver function tests and found a renal lesion. She is otherwise fit and well.

Figure 1.
- What is the sensitivity and specificity of ultrasound (US) for detecting renal tumours? Do you know of any US adjuncts that can improve this?
- What is the best imaging modality for investigating renal cell carcinoma?
- On CT, what change in Hounsfield units may alert you to malignant pathology?
- What are the main limitations of CT / MRI in detecting renal masses with tumour potential?
Case 2
A 65-year-old gentleman presented with visible haematuria and underwent the below CT scan. He has hypertension and hyperthyroidism.

Figure 2.

Figure 3.
- What are the different phases of a CT renal?
- What do Figures 2 and 3 demonstrate? What is the stage of this lesion?
- What are the treatment options for this patient?
Case 3
A 77-year-old gentleman was diagnosed with the below 3cm renal lesion confirmed to be a renal cell carcinoma. Management options were discussed, and he opted for the below intervention.

Figure 4.
1. Can you describe the intervention shown in Figure 4?
2. Please outline the risks involved with this procedure.
Answers
Case 1
1. Sensitivity of US in detecting renal masses depends on the size of the lesion. Sensitivity for tumours >3cm and smaller tumours (2–3cm) is reported to be 85–100% and 67–82% respectively [1]. Plain US typically looks for distortion of architecture. Doppler US identifies increased vascularity to an area relative to the surrounding tissue, which is particularly useful for endophytic tumours and in differentiating between RCC and small angiomyolipomas (AML). Another modality is contrast-enhanced US (CEUS), which identifies areas of renal parenchyma brightness and can assess for microcirculations. CEUS has a suggested sensitivity up to 95% and specificity around 55% [2]. They can help demonstrate hypovascular lesions such as papillary RCC, but may not differentiate RCC from oncocytoma / AML [3].
2. According to the European Association of Urology (EAU) guidelines contrast enhanced multi-phasic CT has high sensitivity (95–100%) and specificity (88–95%) for characterisation and detection of RCC, invasion, tumour thrombus and mRCC [4,5].
3. An increase in 15 Hounsfield units or more in the solid part of a tumour represents enhancement. One systematic analysis reported a median sensitivity and specificity of 88% in identifying renal tumours [6].
4. Limitations of CT include exposure to ionising radiation and nephrotoxic contrast agents, whilst MRI may be contraindicated in patients with metallic prostheses or pacemakers. Historically, it was thought that both CT and MRI were not completely reliable when distinguishing oncocytomas or fat-poor AMLs from renal cell carcinoma. However, a meta-analysis from 2022 concluded that CT had a pooled 83% sensitivity and 92% specificity when differentiating between oncocytomas and RCC [7].
Case 2
1. CT renal consists of multiple phases as outlined below [8]: Non-contrast phase – This is conducted prior to intravenous (IV) contrast administration, with the purpose of detecting calcifications (e.g., renal or ureteric stones) and identifying fat content in mass lesions (e.g., AML). It is also useful in having a baseline attenuation with which to compare the contrast images.Corticomedullary phase – This is conducted approximately 25–40 seconds after contrast injection. Its purpose is to highlight renal arteries, cortex and medulla (the renal cortex enhances preferentially). It is useful in assessing vascular anatomy which can aid surgical planning, and in demonstrating renal artery stenosis / arteriovenous malformations and other abnormalities. It can identify early enhancement in hypervascular tumours.Nephrogenic phase – This is conducted approximately 80–120 seconds after contrast injection. It allows both enhancement of the cortex and medulla and is the best phase for detecting renal masses.
2. This is a 5cm, exophytic, cystic, superior pole tumour of the left kidney, stage T1b N0 Mx.
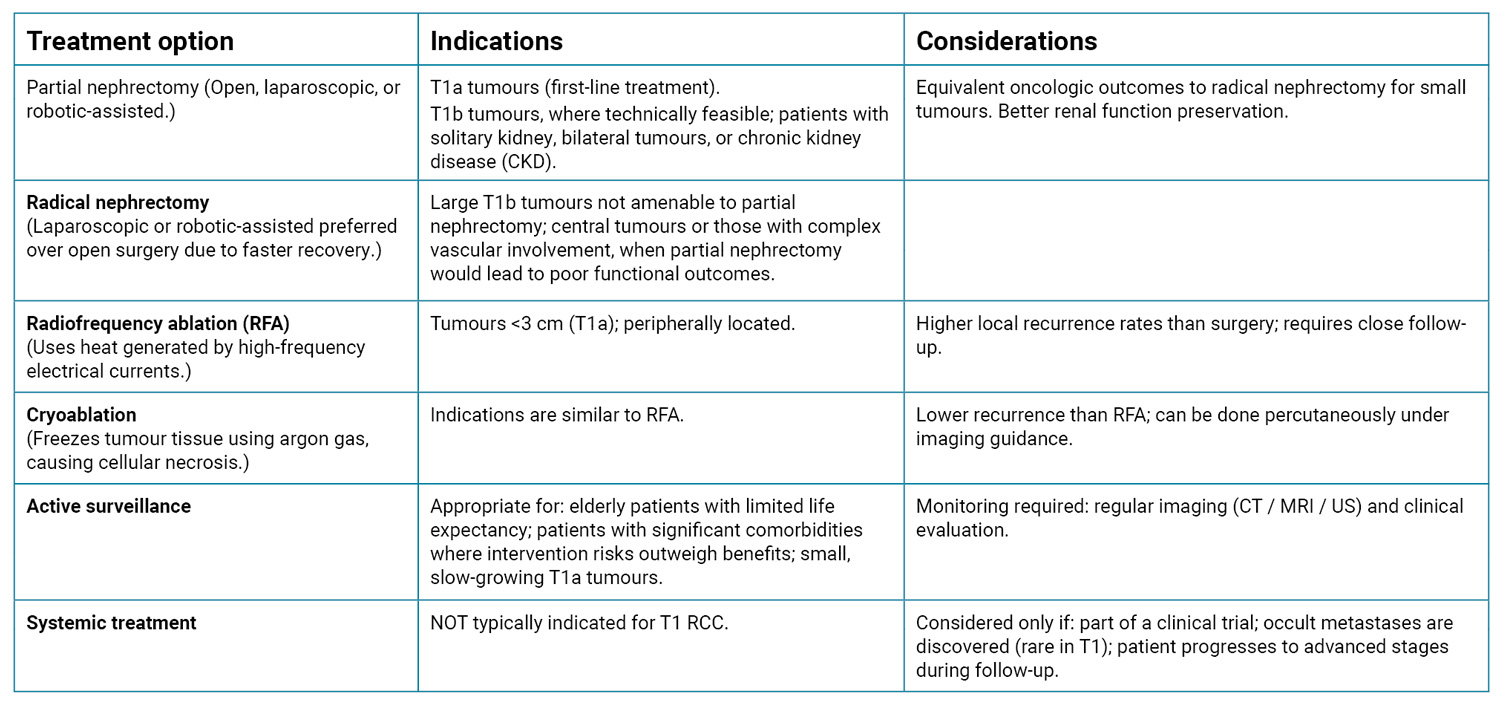
3. A full summary of treatment of these lesions is outlined in the table below [4,9,10].
Case 3
1. This is cryoablation of a small renal tumour.
2. The complications involved with this procedure are listed below, along with their respective risks.

References
1. Rossi SH, Klatte T, Usher-Smith J, Stewart GD. Epidemiology and screening for renal cancer. World J Urol 2018;36(9):1341.
2. Chang EH, Chong WK, Kasoji SK, et al. Diagnostic accuracy of contrast-enhanced ultrasound for characterization of kidney lesions in patients with and without chronic kidney disease. BMC Nephrol 2017;18(1):1–13.
3. Van Oostenbrugge TJ, Fütterer JJ, Mulders PFA. Diagnostic imaging for solid renal tumors: a pictorial review. Kidney Cancer 2018;2(2):79.
4. Ljungberg B, Albiges L, Abu-Ghanem Y, et al. European Association of Urology guidelines on renal cell carcinoma: the 2022 update. European Urology 2022;82(4):399–410.
5. Morshid A, Duran ES, Choi WJ, Duran C. A concise review of the multimodality imaging features of renal cell carcinoma. Cureus 2021;13(2):e13231.
6. Vogel C, Ziegelmüller B, Ljungberg B, et al. Imaging in suspected renal-cell carcinoma: systematic review. Clin Genitourin Cancer 2019;17(2):e345–55.
7. Dehghani Firouzabadi F, Gopal N, Homayounieh F, et al. CT radiomics for differentiating oncocytoma from renal cell carcinomas: systematic review and meta-analysis. Clin Imaging 2023;94:9–17.
8. O’Connor OJ, Maher MM. CT urography. Am J Roentgenol 2010;195(5):W320-4.
9. Finelli A, Ismaila N, Bro B, et al. Management of small renal masses: American Society of Clinical Oncology Clinical Practice Guideline. J Clin Oncol 2017;35(6):668–80.
10. Campbell S, Uzzo RG, Allaf ME, et al. Renal mass and localized renal cancer: AUA guideline. J Urol 2017;198(3):520–9.











