Case 1
A 45-year-old female presents with a one-year history of urinary leakage, especially worse on coughing. She is otherwise well, with no co-morbidities.
- What is the International Continence Society (ICS) definition of stress urinary incontinence (SUI)?
- What are the main findings shown in Figure 1a and 1b?
- How would you evaluate a patient with SUI?
- What are the surgical management options available for the management of SUI?
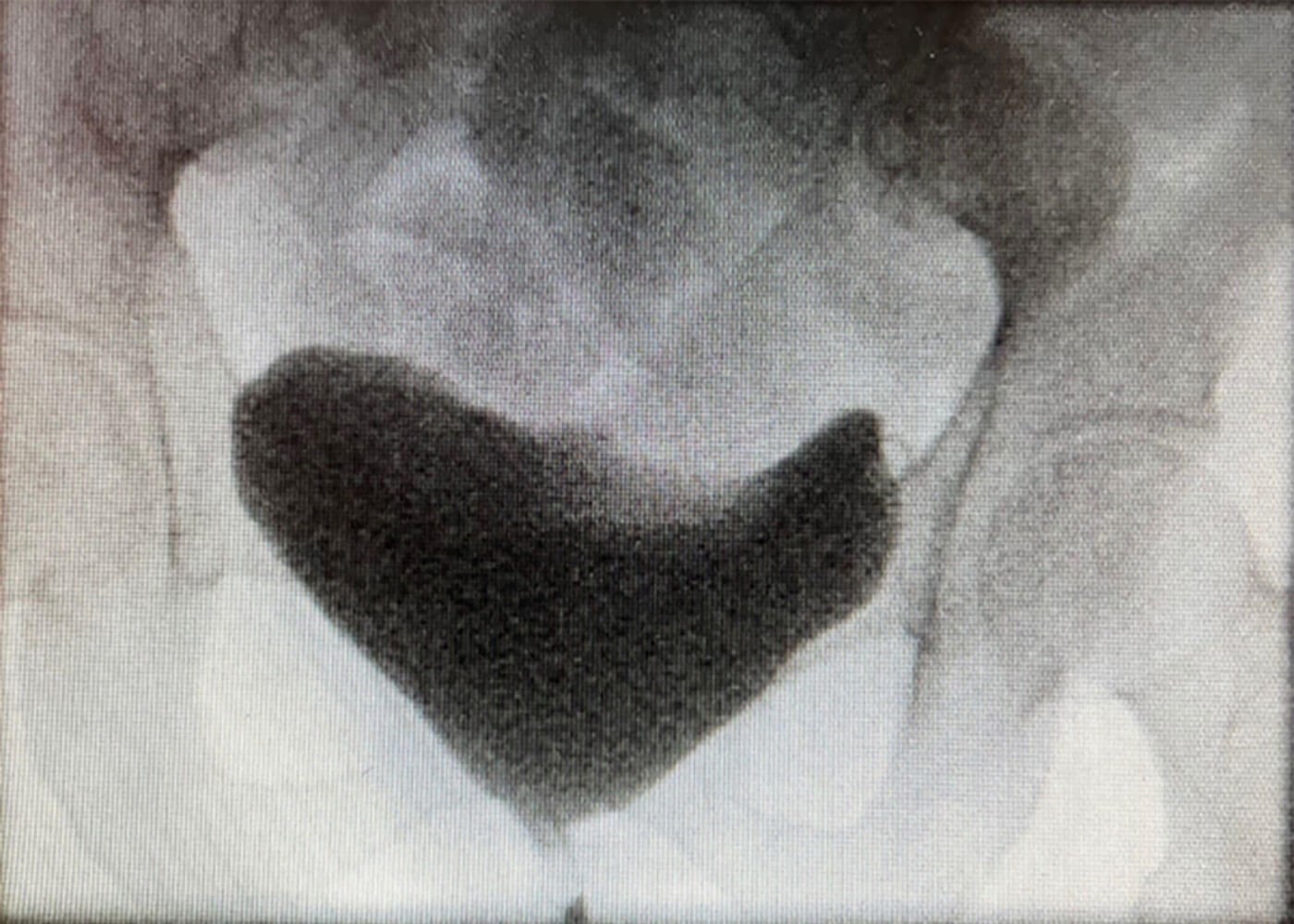
Figure 1a.
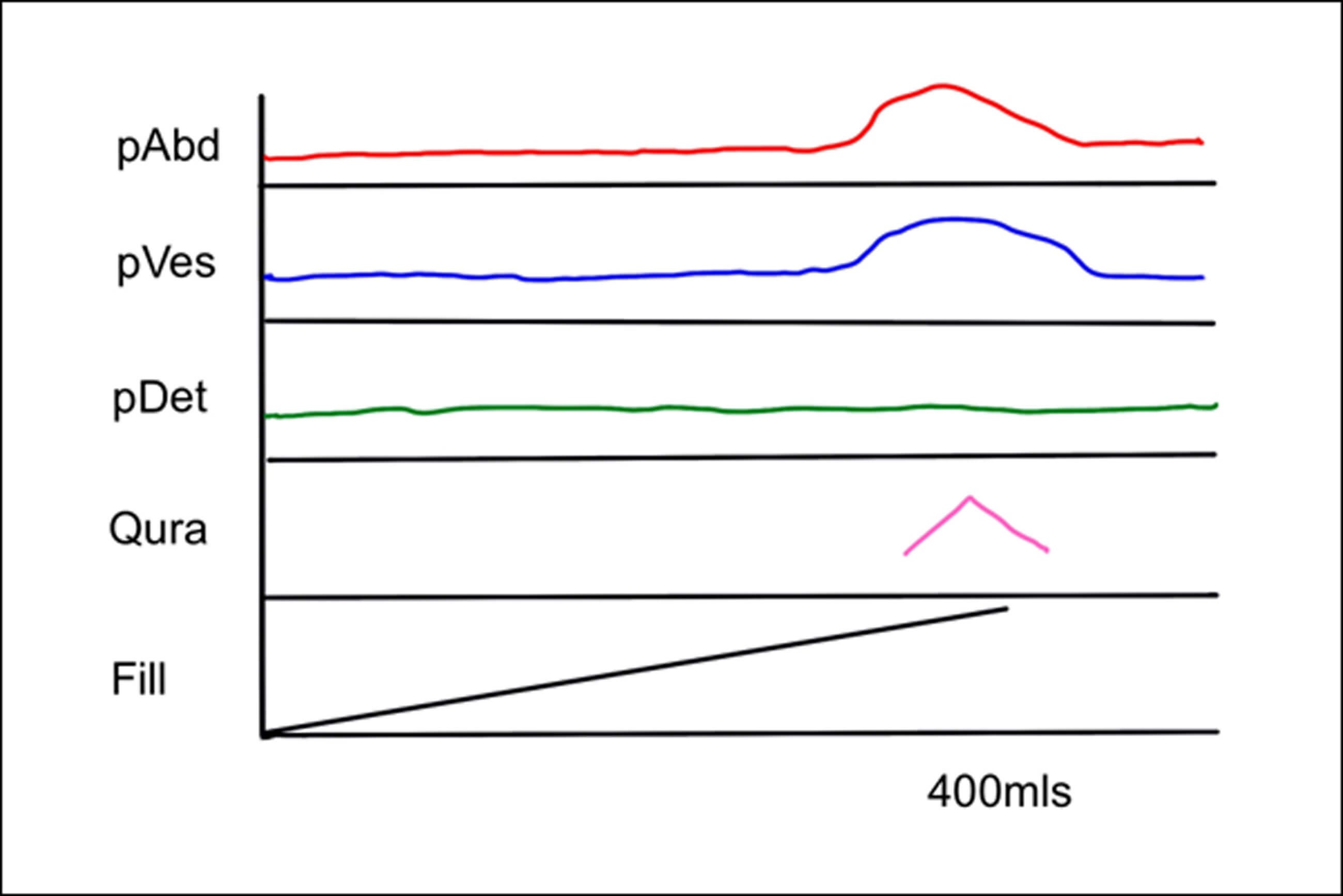
Figure 1b.
Case 2
A 38-year-old female presents with a three-year history of recurrent urinary tract infections (UTIs), dysuria, dyspareunia and a vaginal mass.
1.What is a urethral diverticulum?
2. How do patients with a urethral diverticulum present clinically?
3. How would you investigate a patient with a urethral diverticulum?
4. How would you manage this patient?
Functional and reconstructive urology: answers
Case 1
- SUI is defined by the ICS as “the complaint of any involuntary loss of urine on effort or physical exertion (e.g. sporting activities) or on sneezing or coughing” [1].
- Figure 1a is a video-urodynamic image taken when the patient was asked to cough. It demonstrates leakage of urine on coughing. Figure 1b is a urodynamics trace which shows leakage of urine (pink line) when the abdominal pressure (red line) is raised on coughing while the detrusor pressure (green line) is not raised.
- A thorough history and physical exam in clinic with a urinalysis, post-void residual, validated questionnaire and bladder diary done prior to the consult (as recommended by European Association of Urology (EAU) guidelines on non-neurogenic female LUTS [2]). A standardised cough test should be part of the examination.
- Management options can be divided into non-surgical and surgical. The non-surgical options include lifestyle changes (weight loss, smoking cessation, fluid intake modification), intense pelvic floor exercises with physiotherapist supervision, bladder re-training, vaginal oestrogen if evidence of atrophy and in select cases, duloxetine. Surgical options include bulking agents, mid-urethral slings, artificial urinary sphincters or colposuspension. The management strategy must be tailored to each individual patient.
Case 2
- Female urethral diverticula (UD) are focal fluid-filled, sac-like structures in the peri-urethral tissue invariably communicating with the urethra and expanding the overlying urethral sphincteric tissues over them.
- Patients present in the third to seventh decade of life. Symptoms are variable with the classically described ‘three Ds’ – dysuria, dribbling and dyspareunia – being the most frequent [3]. Other symptoms include frequency, urgency, UTIs and pain. 10-20% of UD are incidental findings on imaging or examination [3].
- After taking a thorough history, a chaperoned physical exam is indicated. The commonest finding in these patients would be an anterior vaginal wall swelling which may be tender if infected. Compression of this mass may extrude a purulent discharge. Smaller diverticula especially those located anteriorly or laterally may not be palpable. A cysto-urethroscopy may reveal the ostium of the diverticulum. Other tests such as ultrasound, voiding cystourethrogram and double balloon positive pressure urethrography have been described but MRI remains the gold standard in diagnosis and surgical planning of urethral diverticula [4].
- The patient should be managed based on the algorithm shown in Figure 2. For symptomatic patients who are fit for surgery, transvaginal excision of the urethral diverticulum with urethral reconstruction is the gold standard procedure with a success rate of >90% [5-7].
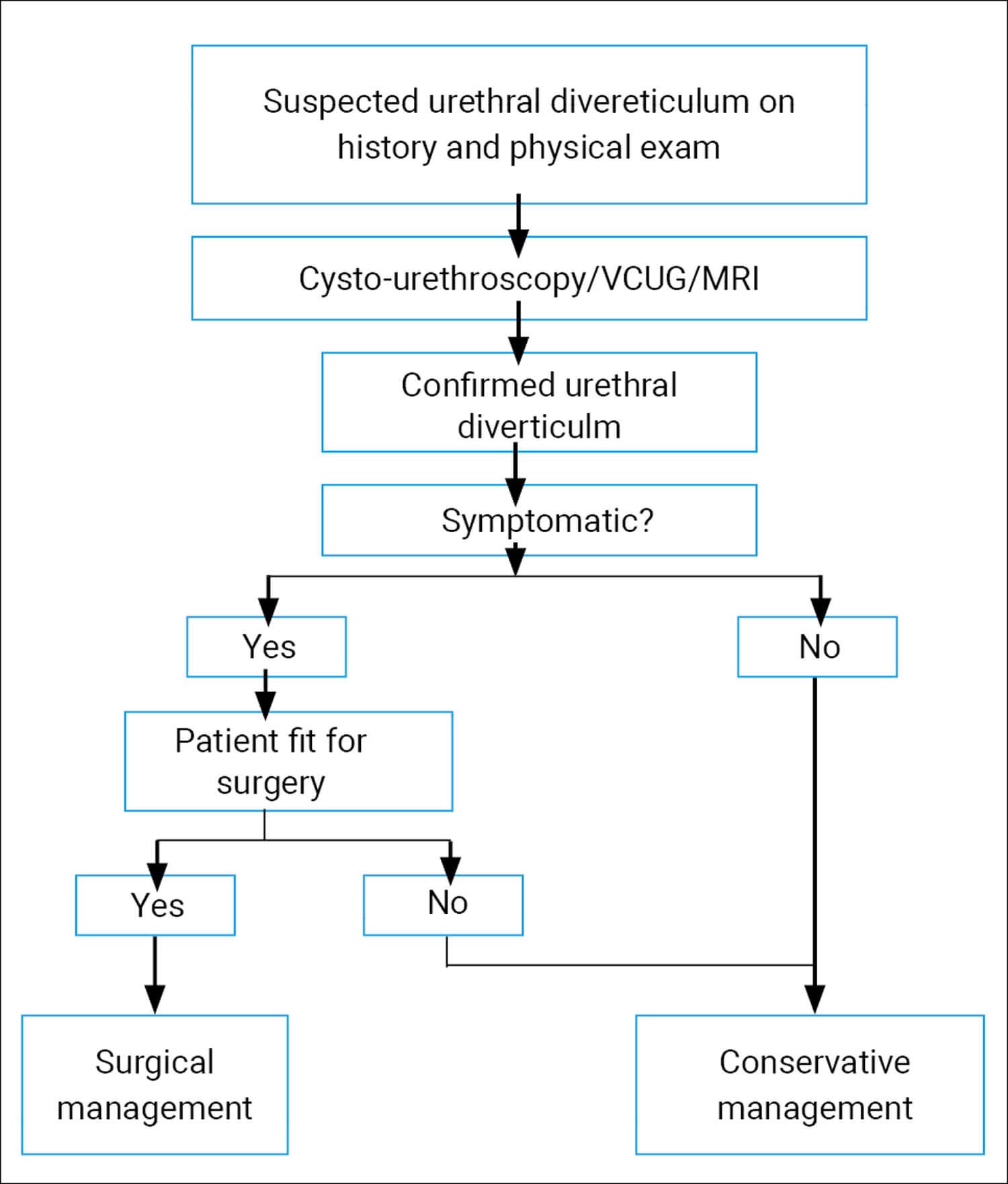
Figure 2: An algorithm for management of urethral diverticula. VCUG – voiding cystourethrography;
MRI – magnetic resonance imaging. Based on EAU Guidelines on non-neurogenic female LUTS [2].
References
1. Haylen BT, de Ridder D, Freeman RM, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn 2010;29(1):4-20.
2. Harding C, Lapitan M, Arlandis S, et al. EAU Guidelines on Management of Non-Neurogenic Female Lower Urinary Tract Symptoms. EAU Guidelines Office; Arnhem, The Netherlands; 2023.
https://uroweb.org/guidelines/non-neurogenic
-female-luts/chapter/introduction
[Accessed 21 March 2023].
3. Baradaran N, Chiles LR, Freilich DA, et al. Female Urethral Diverticula in the Contemporary Era: Is the Classic Triad of the “3Ds” Still Relevant? Urology 2016;94:53-6.
4. Osman NI, Chapple CR. Urethral diverticula. In: Chapple CR, Hamdy FC, Eardley I (Eds.). Oxford Textbook of Urological Surgery Oxford University Press; Oxford, UK; 2017:295-9.
5. Reeves FA, Inman RD, Chapple CR. Management of symptomatic urethral diverticula in women: a single-centre experience. Eur Urol 2014;66(1):164-72.
6. Greiman AK, Rolef J, Rovner ES. Urethral diverticulum: A systematic review. Arab J Urol 2019;17(1):49-57.
7. Crescenze IM, Goldman HB. Female Urethral Diverticulum: Current Diagnosis and Management. Curr Urol Rep 2015;16(10):71.