Case 1
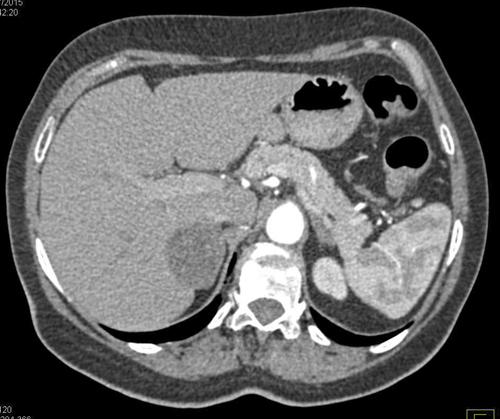
A 45-year-old man undergoes a CT of his abdomen to stage a newly diagnosed bowel malignancy.
- What does the scan show?
- What findings on a CT scan suggest an adrenal lesion is benign?
- If the CT scan is inconclusive, what other imaging modality can be used and what are the common findings with it?
- Given his history, what is the risk of this lesion being benign?
- What percentage of benign adrenal lesions are functional?
- What are the common functional lesions?
- When would you surgically remove an adrenal lesion?
Case 2
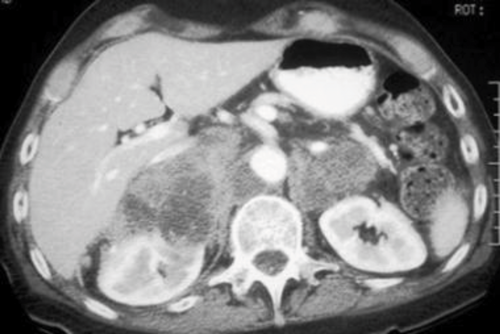
A 78-year-old man presents with shortness of breath and weight loss. As part of his investigations he undergoes a CT of his chest / abdomen / pelvis.
- What does the scan show?
- What is the likely diagnosis?
- What tumours commonly metastasis to the adrenal gland?
- What investigations need to be performed to exclude functionality?
Case 3
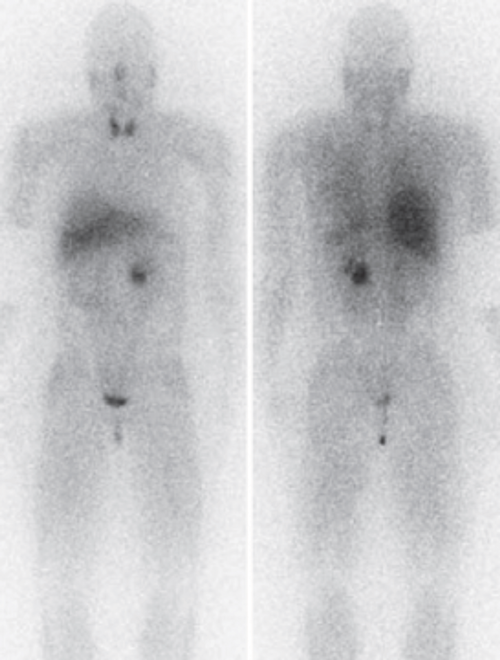
A 35-year-old woman presented to her GP feeling unwell and was found to have an elevated blood pressure of 170/115mmHg. The GP arranged a scan of the abdomen that showed a 3cm adrenal lesion. She is referred to your clinic urgently for review with a suspected phaeochromocytoma.
- What symptoms would you particularly enquire about?
- What is the risk that it is a phaeo?
- It has been called the ‘10%’ tumour; why?
- In view of these risks you perform the shown scan. What is this scan and what does it show?
- Surgery is the treatment of choice. How is the patient maximised preoperatively and what surgical steps are taken to reduce complications?
- Describe the blood supply to the adrenals.
Answers
Case 1
-
An enlarged right adrenal gland, with a smooth contour and homogenous appearance.
-
Smooth, homogenous solitary lesion <4cm with <10HU (i.e. lipid rich), with >60% contrast washout.
-
An MRI scan is as effective as CT for detecting benign from malignant lesions. Non-functional adenoma on T2 imaging have the same density as the liver, with rapid washout of contrast. Malignant lesions show intermediate to high density on T2 imaging, with rapid and intense enhancement.
-
Risk of malignancy is 1%, but given the fact that he has a history of bowel cancer this increases to 75%. Therefore 25% risk it is benign.
-
20%.
-
Cortical lesions – Cushing syndrome, Conn syndrome, sex hormone producing tumour. Medullary lesions: phaeochromocytoma.
-
If functional; If >5cm; If imaging is suggestive of cancer or the lesion increases in size (>5cm) or becomes functionally active during follow-up.
Case 2
-
Bilateral enlarged adrenal glands, with hetrogenous appearance.
-
Bilateral adrenal metastasis.
-
Lung, breast, kidney, colon, melanoma.
-
U&Es for hypokalaemia in Conn syndrome, confirmed by serum renin / aldosterone level. Serum metanephrine for phaeochromocytoma, confirmation by 24 hours urinary metanephrine and vanillylmandelic acid. 24 hours urinary cortisol for Cushing syndrome.
Case 3
-
Headaches (80%), palpitations (65%), sweats (60%), abdominal pains.
-
Phaeochromocytoma account for 5% of adrenal lesions (Cushing 5%, Conn 1%).
-
10% are: bilateral, familial, paediatric, malignant, extra-adrenal. This rule has been challenged as up to 25% are extra-adrenal and up to 30% may be familial.
-
Nuclear medicine metaiodobenzylguanidine (MIBG) scan. Demonstrates a left phaeochromocytoma with no further adrenal or extra-adrenal lesions.
-
Initially needs alpha blockage, with long acting phenoxybenzamine to manage blood pressure. Beta blockers (propranolol) can then be started to prevent cardiac arrhythmias. She will need to be well hydrated preoperatively. Surgically there should be minimal manipulation on the adrenal gland, with early division of the adrenal vein.
-
Arterial supply: superiorly from inferior phrenic artery, directly from the aorta and the ipsilateral renal artery. Left adrenal vein drains into the cranial aspect of the left renal vein. Right adrenal vein enters the inferior vena cava directly on its posterolateral aspect.




