Nephrostomies are a valuable uroradiological intervention which enables drainage of the obstructed kidney, amongst other indications. Complications associated with nephrostomies following placement are not uncommon, with re-presentation to the emergency department or surgical emergency unit. In this review we will focus on indications and contraindications for nephrostomy insertion, troubleshooting common issues and highlighting our own pathway which has been introduced to reduce re-admissions and reduce inpatient hospital stay.
Indications and contra-indications
Insertion of a nephrostomy can be performed in both the elective and emergency setting. Broadly speaking, there are four main indications for percutaneous nephrostomy insertion. These include [1]:
- Relief of urinary obstruction
- Access for therapeutic interventions (including percutaneous nephrolithotomy)
- Urinary diversion
- Diagnostic testing
Whilst there are no absolute contra-indications, patients with severe electrolyte abnormalities such as life-threatening hyperkalaemia (K+ >7mmol/L) refractory to treatment or metabolic acidosis should undergo medical optimisation, which may include emergency dialysis, prior to nephrostomy insertion. Severe coagulopathy should be corrected due to risk of bleeding complications; however, if this is driven by infection it may prove refractory to treatment and therefore requires careful assessment regarding the role of appropriate drainage to control sepsis. In all situations, discussion about benefits, risks and management of the nephrostomy tube is paramount.
The leaking nephrostomy
A stoma bag can be placed around the nephrotomy exit site. If it is not used, the nephrostomy tube can leak from the pigtail connector or nephrostomy exit site onto the skin. A loose connector may only require tightening. Occasionally, the thread in the pigtail nephrostomy tube is too long or sits outside of the drainage system. Using aseptic technique, the connector should be unscrewed, the wire shortened with stitch cutters and re-adjusted back into the tubal system. The tubing should be cleaned with anti-septic wipes and a closed secure system re-established (Figure 1).
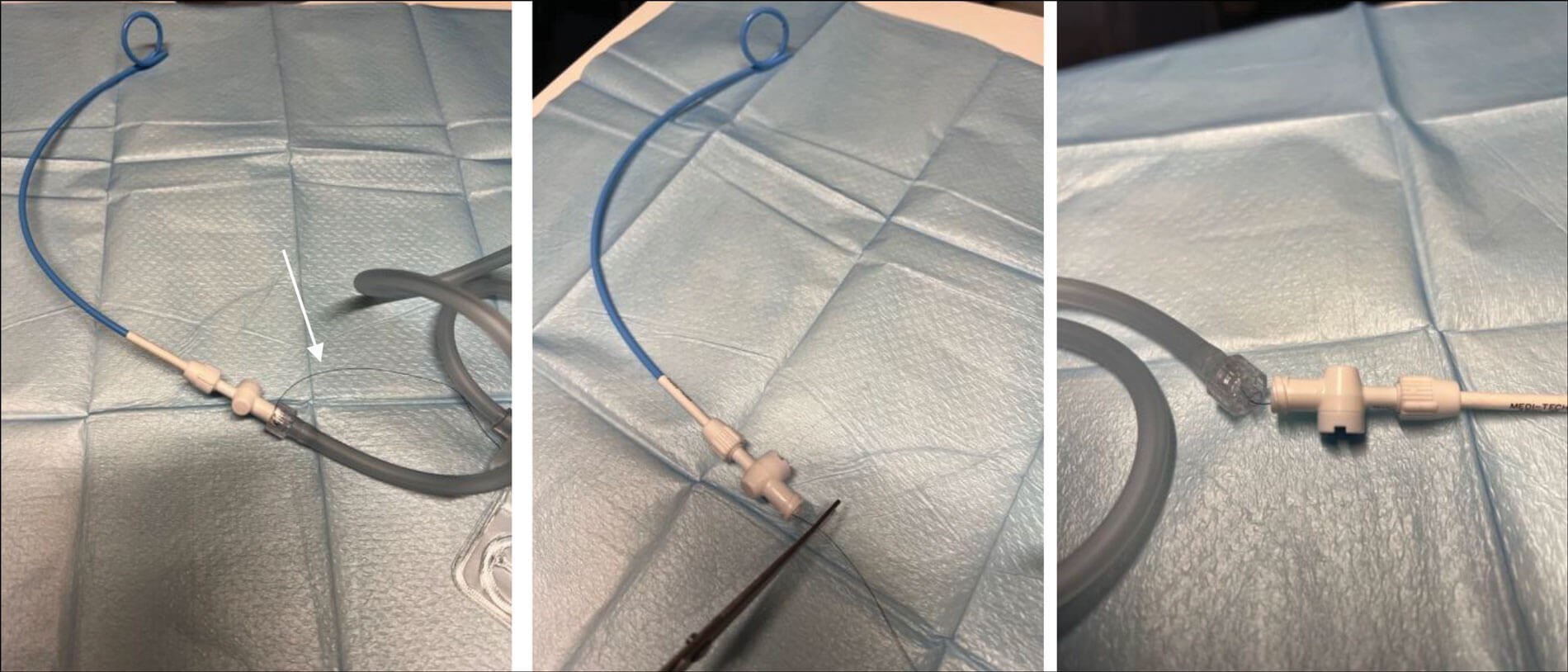
Figure 1: Long pigtail thread sitting outside of the drainage system (marked with white arrow)
which has been shortened and correctly inserted into the drainage tube under aseptic technique.
Leakage from the nephrostomy exit site is frequently seen within seven days of first insertion and requires only absorptive dressings and close monitoring. If this persists after a week, it may be due to kinked or twisted drainage tubing, defective drain bag or a nephrostomy catheter that is smaller than the nephrostomy tract calibre. A twisted or kinked tube should be straightened and secured with a waterproof dressing. A defective drain bag should be replaced.
Where the nephrostomy tract is of wider calibre than the tube a secure dressing should be applied, and the patient given reassurance and education that the tract size will reduce over time.
Persistent leakage is an indication for a nephrostogram (fluroscopic x-ray study) and possible subsequent nephrostomy catheter exchange. In the interim, persistent leakage can be managed with the placement of a stoma bag around the nephrostomy exit site.

Figure 2: Normal pigtail mechanism (left) and failure allowing uncurling of the coil (right).
The dislodged nephrostomy
The nephrostomy tube is held securely in the renal pelvis by a locking pigtail loop. Failure of the locking mechanism (Figure 2) or accidental tugging of the tube can cause partial or entire dislodgement of the tube. If the nephrostomy has fallen out, the patient may have brought the tube with them, which should be inspected. The site should be covered with a sterile absorbent dressing. The indication for nephrostomy should be reviewed and a determination of the continued need for drainage and its urgency should be made. This would include establishment of the history, the original indication for nephrostomy, symptom status and bloods. An example of an urgent indication for nephrostomy reinsertion is an obstructed solitary kidney.
The blocked nephrostomy
The nephrostomy tube can become blocked with debris, blood clots or pus. If there is reduced or no urine draining from the nephrostomy or the patient reports increased pain at the nephrostomy site, the nephrostomy may be blocked and require flushing. If blockage or bypassing occurs frequently, it may be appropriate to flush the tube as a prophylactic measure once or twice a week.
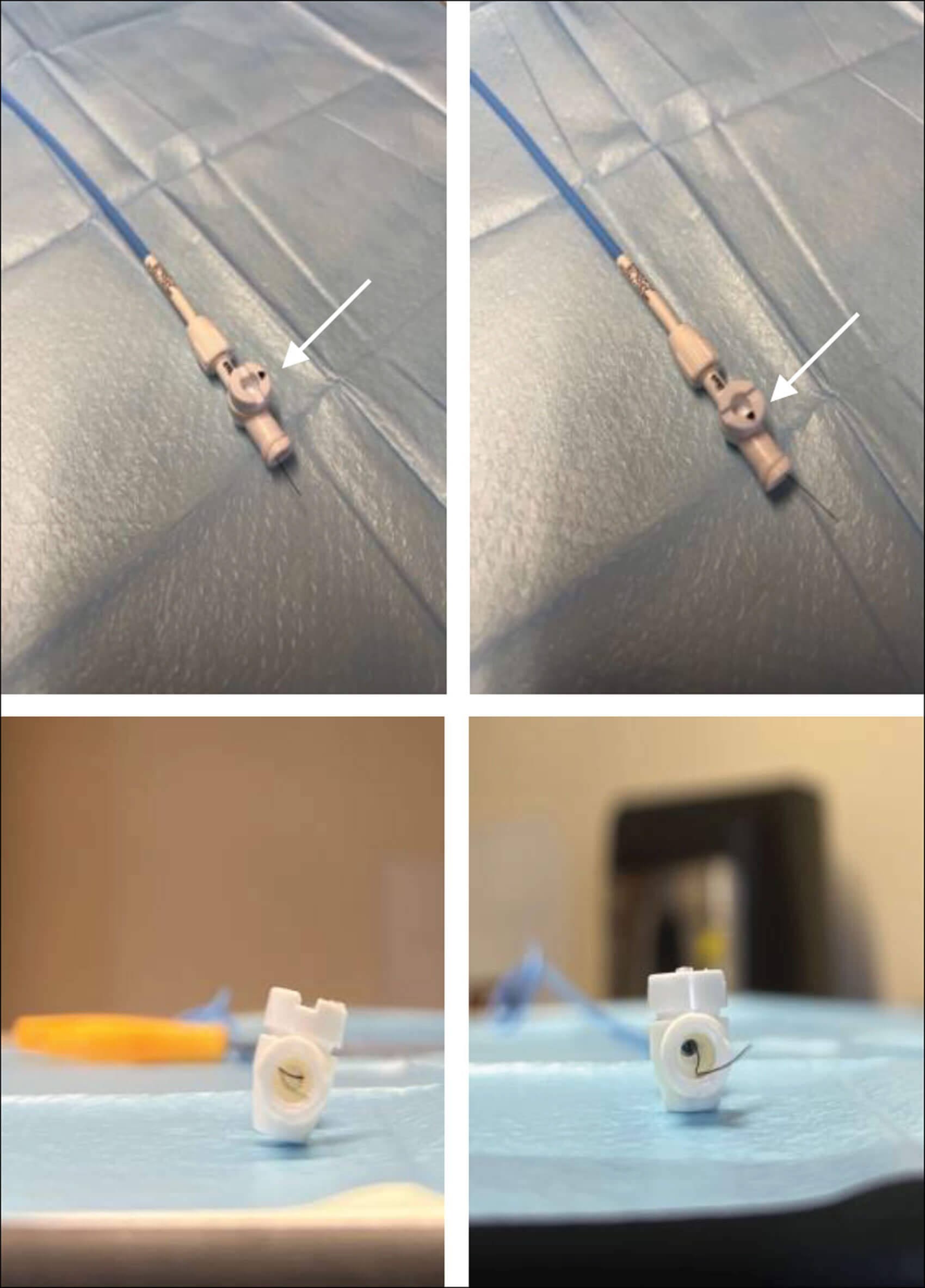
Figure 3: White arrow showing locked nephrostomy tap (left above and below)
and unlocked allowing dislocation of the thread (right above and below).
Flushing the nephrostomy tube
Equipment required:
- Sterile dressing pack (including sterile gloves)
- 10ml syringe
- 10ml sterile 0.9% sodium chloride PosiFlush™
- Chlorhexidine alcohol wipe
- Incontinence sheet and receiver
- Sterile nephrostomy dressing or replacement nephrostomy bag (if used)
- Adhesive removal spray
- Don non-sterile gloves, check the tube and bag to make sure there are no kinks that may be causing mechanical obstruction to the drainage of urine.
- Wash hands.
- Open dressing pack, prepare equipment and draw the normal saline into the syringe.
- Place incontinence sheet underneath the tube and drainage bag.
- Untwist the nephrostomy bag from the drainage tube and place a sterile receiver underneath. It is important not to ‘unlock’ the nephrostomy as it may cause it to dislodge the locking thread (Figure 3).
- Wearing sterile gloves, clean around nephrostomy port with alcohol wipe.
- Attach syringe to port. Gently apply even pressure, instil 5ml normal saline into nephrostomy tube and allow the saline and urine to flow out of the tube.
- If no drainage is observed, this may be repeated with a further 5ml of saline (maximum insertion of saline should never exceed 10ml as the renal pelvis can only hold 5-10ml of fluids).
- If no drainage occurs, gentle aspiration may help to dislodge the clot or stone debris that may be causing the blockage. Expect to withdraw the same 5ml of saline plus urine. If the instilled 5ml cannot be withdrawn, it may indicate that the tube has become unblocked and the fluid is draining down the renal pelvis and ureter. If there is any great resistance, discontinue flushing – NEVER use excessive force when aspirating the tube, this may result in damage to the renal pelvis and cause bleeding.
- Allow the saline and / or urine to flow out of the nephrostomy tube.
- Replace and apply a clear nephrostomy drainage bag ensuring the tube is secure.
- Advise the patient to monitor nephrostomy output for the next four to six hours, if no drainage after flushing the tube, follow the pathway overleaf.
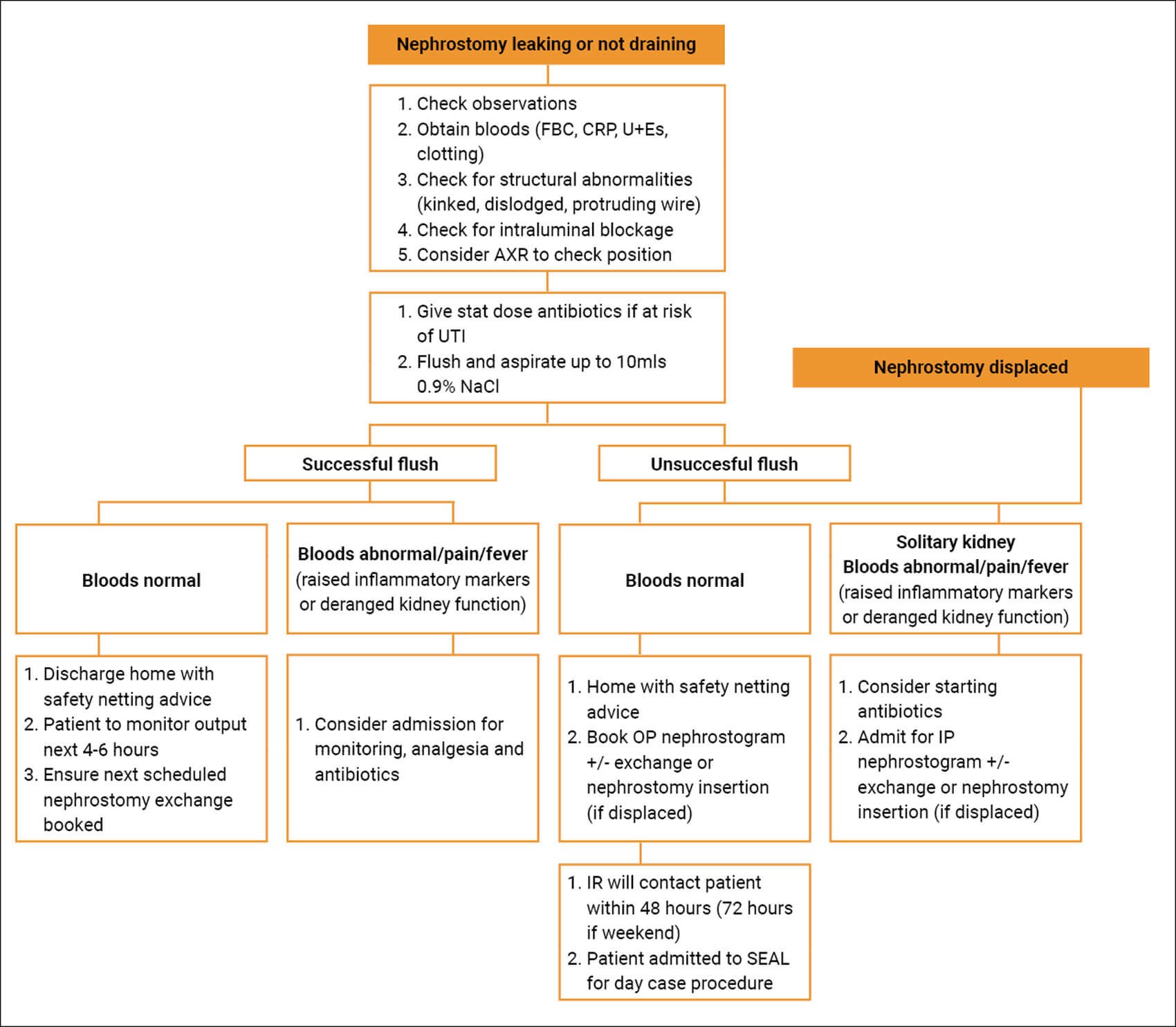
Figure 4: Pathway for ambulatory interventional radiology management of the
non-functioning nephrostomy. IP = inpatient, OP = outpatient, IR = interventional radiology.
Pathway
At our centre where interventional radiology (IR) is based on site we have developed a pathway where patients fulfilling the below criteria are suitable for ambulatory nephrostogram and / or nephrostomy re-insertion (Figure 4):
- Nephrostomy currently or recently in-situ
- Normal observations
- No signs or symptoms of sepsis
- Stable renal function
- Normal clotting
- No or controlled pain.
Patients can be discharged from the emergency department or ward with planned radiology follow-up. An electronic request to IR for a nephrostogram or nephrostomy catheter exchange is placed on discharge. The patient is contacted within 48 hours (72 hours if seen on a weekend) by the radiology department to arrange admission to the surgical elective admissions lounge (SEAL) on the morning of their procedure. They attend fasted and after having their procedure under local anaesthetic are closely monitored for a few hours in the SEAL unit before being discharged. Any subsequent nephrostomy exchanges are booked by the IR department.
Granulation of skin
Granulation tissue at the tube exit site is a normal physiological reaction. Securing the tube with a dressing can avoid associated pressure injury and movement. If there is associated bleeding topical silver nitrate cautery can be utilised in the clinic or ward setting.
Post-obstructive diuresis
A previously obstructed kidney may produce high volumes of urine once the obstruction is relieved. Diuresis is defined as urine output >200ml/hr for two consecutive hours [2]. Prolonged polyuria >48 hours is pathological and can result in dehydration, hypotension, hypovolaemic shock and electrolyte imbalance if untreated. The patient requires admission for daily electrolyte monitoring with hourly fluid input and output balance charts. Oral fluid replacement should be commenced at 50% of urine output. Intravenous fluid replacement is indicated for postural hypotension, haemodynamic instability, correction of severe electrolyte disturbances or if the patient is unable to meet their oral fluid requirement [3].
Infection and sepsis
Low-grade fever is common immediately following nephrostomy tube insertion. This may be secondary to inflammatory mediators released during the procedure. Progression to septic shock occurs in 1-3% of cases [4]. Due to the high mortality, risk prevention is key, and antibiotics should be given pre-procedure and considered post-procedure. Where purulent urine is seen, a sample should be obtained for microscopy, culture and sensitivity, and post-procedure antibiotics given. Close monitoring for signs and symptoms of sepsis is essential, with an awareness that in some cases high dependency unit (HDU) or intensive therapy unit (ITU) care for cardiovascular and respiratory support may be required.
Patients frequently present to the emergency department with signs and symptoms of upper and lower urinary tract infections (dysuria, bleeding, flank pain and fevers). Following an initial Accident & Emergency assessment, patients should be appropriately resuscitated and treated with antibiotics based on previous sensitivities. A gentle flush with 5–10ml 0.9% NaCl should be performed if there is reduced or no drainage into the nephrostomy bag. Bloods should be obtained and those with abnormal renal function may require an abdominal x-ray to confirm the position of the tube. A nephrostogram confirms both position and patency of the tube. Where upper urinary tract infection is suspected, an inpatient or outpatient nephrostomy catheter exchange is performed once the patient is stable and the infection has been treated.
References
1. Dagli M, Ramchandani P. Percutaneous nephrostomy: Technical aspects and indications. Seminars in Interventional Radiology 2011;28:424‑37.
2. Shah A. A guide for the assessment and management of post-obstructive diuresis. Urology News 2015;19(3):15-17.
3. Stephen LW, Sajjad H, Sharma S. Postobstructive diuresis. StatPearls [Internet] 2022
https://www.statpearls.com/
point-of-care/38132
[last accessed 16 November 2023].
4. Ramchandani P, Cardella JF, Grassi CJ, et al. Quality Improvement Guidelines for percutaneous nephrostomy. Journal of Vascular and Interventional Radiology 2001;12:1247-51.
Declaration of competing interests: None declared.