Case scenario
A 45-year-old male presents to Accident & Emergency with two days of intermittent, severe, left-sided loin to groin pain and multiple episodes of vomiting. He undergoes imaging as part of his investigations.

Figure 1.

Figure 2.
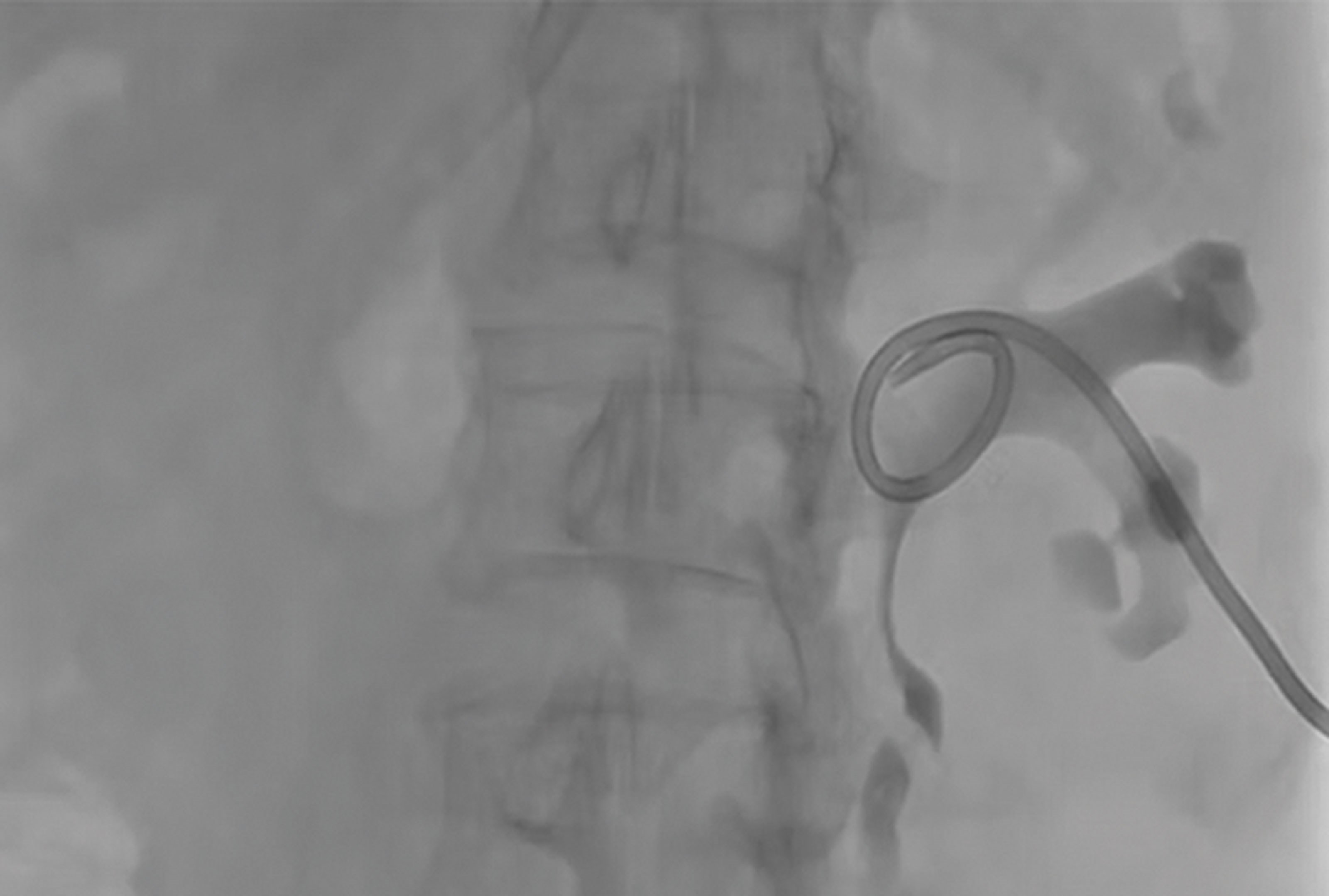
Figure 3.
- Describe Figure 1 and the acute urological diagnosis.
- Which features typically seen in upper urinary tract obstruction are demonstrated in Figure 2?
- A+E doctors review the patient following the CT, where he complains of worsening pain associated with a temperature of 38.7 degrees and heart rate of 114. He is referred to the urology department. What are the management options for this patient? What evidence do you know to support your decision?
- Describe Figure 3. What are the contraindications to and possible complications of percutaneous nephrostomy insertion?
Answers
1. This is a coronal reconstruction of an unenhanced low dose CT of kidney, ureter, bladder (KUB) in the soft tissue window which demonstrates a 7mm (craniocaudal length) left upper ureteric calculus with mild upstream hydroureteronephrosis and associated periureteric fat stranding.
2. The corresponding axial image at the level of the renal hilum, with the patient scanned in the prone position, shows signs of obstruction: (mild) left hydronephrosis with associated perinephric fat stranding and small amount of perinephric fluid.
3. The different management options are:
- Conservative management: In the absence of risk factors including, but not limited to, active urinary tract infection (UTI), obstructed single kidney, significant acute kidney injury (AKI) or intractable pain, conservative management may be considered. The MIMIC calculator can be used to predict the likelihood of spontaneous stone passage (SSP) [1]. In this case, including the use of medical expulsive therapy, the chance of SSP is quoted at only 20–30%. Given the presence of an infected obstructed kidney along with stone size and location, a conservative trial would not usually be considered appropriate for this patient.
- Insertion of a retrograde ureteric stent: If emergency acute decompression of the collecting system is indicated, rigid cystoscopy and placement of retrograde ureteric stent (commonly performed under general anaesthetic) can be considered followed by definitive stone management at a later date. A temporary stent insertion is only typically indicated when an obstructed stone is associated with risk factors, such as those stated above.
- Insertion of percutaneous nephrostomy (PCN) +/- antegrade (AG) ureteric stent: If urgent decompression is required and there is concern over the patient’s suitability for general anaesthesia, then insertion of a PCN can be considered if available in a timely fashion. This can offer a prompt and relatively safe temporising method of drainage of the affected kidney with a plan for secondary definitive stone management. Consideration of an AG stent insertion can be given at the time of nephrostomy insertion however caution should be taken in the context of an infected system as additional intervention can worsen the patient’s clinical picture acutely.
This patient has evidence of an infected obstructed urinary system. Most clinicians would agree this patient requires prompt kidney drainage which can be achieved via retrograde ureteric stenting or PCN insertion. If available in a suitable timeframe locally, and in the absence of contraindications, you may consider PCN preferentially due to the presenting associated features concerning for urosepsis. Pearle and colleagues produced a seminal paper in 1998 comparing the two methods of drainage in an infected obstructed kidney secondary to a ureteric calculus and found neither modality demonstrated superiority in promoting a more rapid recovery. Time to both temperature and white blood count normalisation was comparable in both groups and there was no significant difference in length of hospital stay [2].
4. Figure 3 shows a fluoroscopic image of a left percutaneous nephrostomy tube. There are no absolute contraindications to PCN insertion. Relative contraindications include:
- Uncorrected bleeding diathesis / coagulopathy.
- Severe electrolyte abnormalities (K+ >7) or metabolic acidosis; whilst nephrostomy insertion is ultimately required to correct these abnormalities, these patients should undergo medical optimisation, which may include haemodialysis / filtration prior to nephrostomy insertion.
- Uncontrolled hypertension.
- Uncooperative patient [3].
Below is a list of possible complications that should be included in consenting for PCN insertion:
- Severe bleeding.
- Vascular injury requiring embolisation or nephrectomy.
- Damage to adjacent structures; liver, bowel, spleen.
- Urine leak / urinoma.
- Pneumothorax.
- Worsening sepsis.
- Failed insertion.
- Tube displacement / blockage [3].
References
1. Shah T, Chuanyu G, Peters M, et al. Factors associated with spontaneous stone passage in a contemporary cohort of patients presenting with acute ureteric colic: results from the Multi-centre cohort study evaluating the role of Inflammatory Markers In patients presenting with acute ureteric Colic (MIMIC) study. BJU International 2019;124(3): 504–13.
2. Pearle MS, Pierce HL, Miller GL, et al. Optimal method of urgent decompression of the collecting system for obstruction and infection due to ureteral calculi. The Journal of Urology 1998;160(4):1260–4.
3. Dagli M, Ramchandani P. Percutaneous nephrostomy: technical aspects and indications. Seminars in Interventional Radiology 2011;28(4):424–37.











