For Part 1 of this topic is available here.
The major limitations of the transrectal ultrasound (TRUS) guided prostate biopsy (PBx) protocols are the risk of profound sepsis and the risk of persistently significant false negative rates, related to the under sampling of the anterior and apical prostate. To address these limitations, transperineal (TP) PBx has had a resurgence in routine clinical practice in the UK, ushering in the modern era of PBx.
From the earliest days of open perineal PBx under general anaesthesia (GA), to the most modern ultrasound guided free-hand transperineal PBx under local anaesthesia (LA), the journey of the evolving PBx techniques appears to have gone full circle to where it all started!
Transperineal ultrasound (US) guided prostate biopsy
TP PBx via US guidance was first described in 1981 [1]. US-guided PBx via the TP route was then reported in 1994, for a patient in whom the transrectal approach was unsuitable [2]. A more recent study reported a cancer detection rate of 82% using TP PBx on patients with elevated prostate specific antigen (PSA) and previous abdominoperineal excision [3]. US-guided TP PBx was developed further, due to the key advantage that the TP approach has a far better sampling of both the anterior prostate [4] and the apical region [5], in addition to the low risk of sepsis. A 2005 paper pointed out the importance of obtaining a large number of cores in TP PBx to improve the cancer detection rate [6].
However, this is affected by differing prostate volumes. Ficarra’s study found that in volumes less than 30cc, a scheme including as low as eight peripheral cores was not statistically different to higher core schemes, however this difference became greater with larger volumes. Over 50cc, a 14-core scheme was still considered to be inadequate, therefore even more cores were recommended for larger prostate volumes [5]. The perceived need for more biopsies led to the systematic TP biopsy using the brachytherapy grid.
Transperineal template prostate biopsy
An adapted method of the TRUS-guided TP PBx is that which uses a template to guide sampling of the prostate. This systematic method gives increased analysis of the whole prostate and reduces the randomness of the original multiple core method, particularly allowing coverage of the apical and anterior regions as mentioned above. A 2001 study found that a repeat biopsy using the TP template, on patients with clinically suspected prostate cancer (PCa) but previous negative biopsy, found cancer in 43% of cases [7]. Since then TP template PBx has been extensively evaluated in numerous studies.
The emergence of focal ablation as a therapeutic option for PCa has increased the need for reliable and accurate localisation of tumours within the prostate – both sextant and extended TRUS-guided TR PBx schemes have been shown to be severely limited in this regard. Whilst the 12-core extended TRUS PBx method was seen to increase the overall accuracy somewhat versus the sextant method, it was still concluded to be an unsuitable diagnostic test for focal therapy selection [8].
These limitations have led to further evolution of the TP approach using a fixed brachytherapy grid and mapping the prostate gland in three dimensions. This allows PCa to be better localised and defined within the grid, in order to select patients to be later treated via focal ablation therapy [9-11]. Grids of different specifications have been evaluated, with a 5mm grid proving to be better for cancer detection than a 10mm grid, producing a rate of 75% cancer detection over 33% from the larger 10mm grid [12]. In a 2009 report, patients with unilateral disease diagnosed by TRUS guided PBx, then undergoing restaging using the TP method of mapping (median 50 cores) before focal therapy, were found to have bilateral cancer in 61% of cases and upgrading in 23% [13].
A 2015 study comparing the accuracy of TP template PBx with TRUS PBx found that template PBx more accurately predicted clinical risk category, and it was recommended that before active surveillance (AS) was commenced, a template PBx should be considered to confirm suitability for AS and that occult higher risk disease had not been missed. TP template PBx has also earned a definite place in the AS protocol for PCa in many centres, whilst following up such patients, and this approach has been further enhanced by the introduction of multi-parametric (mp) MRI [14].
Despite the relatively high pick up rate of significant disease and better characterisation of low-risk disease, the risks of bleeding and retention of urine of over 10% were common with the elaborate template mapping PBx [15,16]. A modified method called ‘sector mapping’ PBx was introduced, whereby tissue cores were only obtained from the peripheral zone (PZ) of the prostate on either side, dividing the PZ into anterior, middle and posterior sectors. This scheme avoids the transition zone where isolated PCa is rare but bleeding commonly seen. In addition, in prostates >30cc volume, biopsies were also taken from the base of the prostate on either side.
Limiting the cores taken reduced the morbidity for patients, speeded up the biopsy and pathology reporting process, without compromising the detection rate of significant cancer [17-19]. The predictive ability of TP sector mapping PBx is improved further when using MRI based PSA-density in selecting appropriate patients [20].
The limitations of these various types of TP mapping PBx are: the need for GA, the subsequent pressure on day surgery waiting lists, and potential delays in the cancer diagnostic pathways, not infrequently seen within a service such as the NHS. MRI-guided prostate biopsy MRI scanning provides much higher spatial resolution than ultrasound, and volumetric imaging capabilities in multiple planes. In addition to the commonly available 1.5-Tesla magnets, the 3-Tesla magnets have well improved the resolution of mpMRI [21].
The earlier techniques of incorporating MRI into PBx involved taking the PBx in-bore in the MRI scanner. In a study by Roethke et al., of patients with only previous negative TRUS biopsy, the cancer detection rate was 52%, of which 19.2% were clinically insignificant [22]. However, in-bore biopsies were found to be severely limited by patient discomfort, long procedure durations, high cost, lack of expertise, the need for specialist equipment, and a sophisticated radiology department in which to perform the biopsy.
Whilst the TR approach was generally favoured, a TP technique was also proposed. As MRI-guided brachytherapy for PCa developed and became more technologically advanced, an in-bore MRI-guided TP PBx programme was introduced where the prostate and suspicious lesions were sampled in a real-time directed fashion [23,24]. A detection rate of 30% was reported. Additionally, a separate study showed the accuracy of MRI targeting of prostatic lesions to be high, with 95% needle placement errors being less than 4mm [25]. The greatest problem is the need for systematic biopsy in addition to the targeted biopsy.
MRI cognitive-targeted biopsy
The difficulties of in-bore PBx led to the transfer of MRI information to TRUS PBx. Cognitive fusion guidance was the first of this type, in which the MRI is used to identify lesions initially and then, after reviewing the MRI images, the urologist attempts to manually guide a biopsy needle to that predetermined location using TRUS guidance. However, the transverse plane slightly differs between MRI and TRUS, hence this required significant experience and training, and results were highly inconsistent. Sensitivity and specificity of 95% and 100% were reported for the cognitive targeted biopsy, over the respective 95% and 83% of extended / mapping biopsy schemes. Additionally, cognitive targeted PBx had a 16% increased rate of high-grade tumour detection [26].
MRI-TRUS fusion biopsy
MRI-TRUS fusion biopsy was the next advance in this technology and is currently rapidly developing, in which, again, an MRI is first taken separately but the MRI image is fused with a 3D ultrasound image. When the TRUS probe moves, the fused MRI image also moves in the same way allowing the urologist to use the MRI image within a TRUS-guided PBx technique. The overall cancer detection rate was found to be 62.9%, with 14.3% being detected only by MRI-TRUS fusion PBx [27]. A later development in 2014 included the use of a mechanical arm holding and detecting the TRUS probe’s positions, instead of the original device which used free-hand electromagnetic trackers.
A study compared the effectiveness of this modified device against clinically guided biopsy. The mechanical arm fusion had positively improved results, including an increase of 11.7% cancers detected [28,29]. The fusion biopsy was further modified, with no mechanical arm tracking or GPS tracking, instead allowing free-hand use of the TRUS probe under spatially combined MRI and TRUS imaging only. This method was seen to significantly improve cancer detection against the systematic 12-core TRUS method [30]. The tumour detection rate was 52% [31]. The superiority of MRI-TRUS fusion targeted PBx over systematic TRUS PBx in finding clinically significant cancer (38% vs. 26%) was yet again confirmed by the most recent multicentre PRECISION study [32].
Combination of MRI targeted and systematic biopsy
The importance of combining MRI targeted PBx with systematic PBx was elegantly demonstrated in a recent multicentre study where the significant PCa (Gleason 7–10) detection rate was 71% when a combination of targeted and systematic PBx was used in 418 biopsy naïve men with high grade MRI lesions (PI-RADS 4–5), in comparison to only 59% significant PCa detection rate, when only targeted biopsies were taken from these lesions [33].
Elastography - enhanced ultrasound techniques
The mechanical properties of cancerous changes to prostate tissue such as increased stiffness can be assessed by ultrasound and MRI-based elastography [34]. Ultrasound-based sonoelastography (RTE) is a recent technique used to aid PBx. The targeted RTE technique has shown a superior per-core cancer detection rate to randomised TRUS-guided PBx, shown in both repeat biopsy as well as first-time biopsy patients [35]. However, when comparing RTE only (without targeting) to the randomised standard technique, the standard technique detected more than three times the number of cancers, implying a potential supplementary role for RTE as opposed to a replacement.
In the largest randomised controlled trial (RCT) to-date, of 353 patients with clinical suspicion of cancer, the RTE group had a superior cancer detection rate of 51% to 10-core TRUS-guided which had 34%; however it was concluded that the overall sensitivity remained low [36]. Further developments in this field include, ‘shear-wave elastography’ (quantitative evaluation of the tissue performed by a generated and defined shear-wave), ‘doppler ultrasound system’ (imaging tumour neovascularisation in order to detect PCa) [37] and ‘HistoScanning™’. HistoScanning is an US-based technology which uses computer-aided analysis to quantitatively describe the malignant disorganisation of prostate tissue, and is thought to have potential to describe cancer foci non-invasively. However, evidence for these new techniques is currently limited, leaving their clinical relevance unclear [38].
Ultrasound guided, free-hand transperineal biopsy
Brachytherapy stepper units and template grids increase costs and operative times for the practising urologist, in addition to the need for a GA taking prostate diagnostics away from the office setting. Moreover, prostates >100cc may be outside the confines of the brachytherapy template making sampling difficult and less precise. Ultrasound guided free-hand transperineal (US-FH-TP) PBx as an alternative option has been pioneered by urologists in Japan, Italy, USA and Australia [39].
Although this approach allows biopsies to be done quite easily under LA, it is still quite difficult to access the anterior apex and guidance of the needle in line with the ultrasound view can be challenging. Despite these limitations, the principle of free-hand TP PBx has great merit and excellent results can be achieved. A total of 274 US-FH-TP PBx were performed in 244 patients by Allaway’s group (2016). Operative and total operating room use times were 7.9 and 17.5 minutes, respectively, with an average of 14.4 cores obtained during each procedure. The overall cancer detection rates for all procedures, those in biopsy naïve patients and those performed for Active Surveillance were 62.8%, 56.4% and 89%, respectively.
New diagnoses of prostate cancer occurred in 41.2% of patients with 10% positive after a previous negative TRUS guided biopsy. Complications including systemic infection, urinary retention and haematuria or pain requiring physician or hospital intervention did not occur [40]. The same group further performed US-FH-TP PBx under LA (2016) in 33 patients. They reported that the procedure was well tolerated by all patients. However, some patients reported bladder discomfort when obtaining cores from the anterior horn. The mean procedural time was 9.19 ± 3.54 minutes with a mean number of 12.94 ± 3.38 cores taken per biopsy [41].
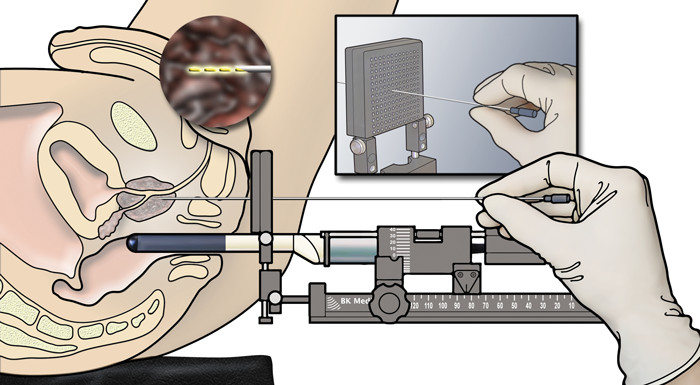
Figure 1. Transperineal template prostate biopsy with transrectal ultrasound guidance.
© BK Ultrasound
The most recent development has been the PrecisionPoint™ Transperineal Access System which facilitates free-hand TP PBx under LA (Figure 1). The advantage of this device is that the perineal access needle is linked via a carriage system which clamps to a linear array probe and keeps the biopsy guide in line with the US transducer. This facilitates better cognitive targeting of identified lesions as well as a more comprehensive systematic biopsy. The device has FDA approval and has just achieved its CE mark. It is likely to be an effective approach for TP PBx under LA in the outpatient setting. Preliminary data reported at the BAUS Oncology Annual Meeting 2017 is encouraging [42].
Figure 2: PrecisionPoint™ transperineal access system (Perineologic).
The future
There are some new techniques which featured in a recent EAU meeting including, ultrasound CT with artificial intelligence (AI-US-CT) targeted biopsy [43], a novel robotic device – the iSR’obot Mona Lisa – to perform MR-US fusion TP PBx [44] and the Trimodal (18)F-Choline-PET / mpMRI / 3D -TRUS targeted PBx [45]. We will have to wait and see how these evolve into day-to-day clinical practice.
As far as diagnostic prostate biopsies are concerned, the Holy Grail would be free hand transperineal MRI–US fusion PBx under LA in the outpatient setting and it may be within our grasp. Such systems would make use of currently available electromagnetic localisation systems and incorporate the available US–MR fusion software to provide better targeted biopsies, but also effective systematic biopsies from the apparently normal peripheral zone whilst minimising the risk of sepsis.
In the meantime, using combinations of screening tests and risk calculators are proving useful in allowing those patients with predominant benign and low risk disease to be reassured without the need for biopsy, as well as better predicting the possibility of diagnosing clinically significant PCa [46].
Declaration of competing interests:
Rick Popert receives Honoraria and meeting support from BXT-Accelyon, the global distributor of the Precision Point Device and from BK Ultrasound.
References
1. Holm HH, Gammelgaard J. Ultrasonically guided precise needle placement in the prostate and the seminal vesicles. Journal of Urology 1981;126:385.
2. Filderman PS, Jacobs SC. Prostatic ultrasound in the patient without a rectum. Urology 1994;43(5):722-4.
3. Shinohara K, Gulati M, Koppie TM, Terris MK. Transperineal prostate biopsy after abdominoperineal resection. Journal of Urology 2003;169(1):141-4.
4. Demura T, Hioka T, Furuno T, et al. Differences in tumor core distribution between palpable and nonpalpable prostate tumors in patients diagnosed using extensive transperineal ultrasound‐guided template prostate biopsy. Cancer 2005;103(9):1826-32.
5. Ficarra V, Martignoni G, Novella G, et al. Needle core length is a quality indicator of systematic transperineal prostate biopsy. European Urology 2006;50(2):266-71.
6. Yamamoto S, Kin U, Nakamura K, et al. Transperineal ultrasound-guided 12-core systematic biopsy of the prostate for patients with a prostate-specific antigen level of 2.5–20 ng/ml in Japan. Int J Clin Oncol 2005;10(2):117-21.
7. Igel TC, Knight MK, Young PR, et al. Systematic transperineal ultrasound guided template biopsy of the prostate in patients at high risk. Journal of Urology 2001;165(5):1575-9.
8. Tsivian M, Kimura M, Sun L, et al. Predicting unilateral prostate cancer on routine diagnostic biopsy: sextant vs extended. BJU International 2010;105(8):1089-92.
9. Barzell WE, Whitmore WF. Transperineal template guided saturation biopsy of the prostate: Rationale, indications, and technique. Urology Times 2003;31(5):41‑2.
10. Barzell WE, Melamed MR. Appropriate patient selection in the focal treatment of prostate cancer: the role of transperineal 3-dimensional pathologic mapping of the prostate - a 4-year experience. Urology 2014;70(6):S27-S35.
11. Sartor AO, Hricak H, Wheeler TM, et al. Evaluating localized prostate cancer and identifying candidates for focal therapy. Urology 2008;72(6):S12-S24.
12. Crawford ED, Wilson SS, Torkko KC, et al. Clinical staging of prostate cancer: a computer‐simulated study of transperineal prostate biopsy. BJU International 2005;96(7):999-1004.
13. Watanabe M, Hayashi T, Tsushima T, et al. Extensive biopsy using a combined transperineal and transrectal approach to improve prostate cancer detection. International Journal of Urology 2005;12(11):959-63.
14. Scott S, Samaratunga H, Chabert C, et al. Is transperineal prostate biopsy more accurate than transrectal biopsy in determining final Gleason score and clinical risk category? A comparative analysis. BJU Int 2015;116 Suppl 3:26-30.
15. Rosario DJ, Lane JA, Metcalfe C, et al. Short term outcomes of prostate biopsy in men tested for cancer by prostate specific antigen: prospective evaluation within ProtecT study. BMJ 2012;344:d7894.
16. Challacombe B, Dasgupta P, Patel U, et al. Recognizing and managing the complications of prostate biopsy. BJU International 2011;108(8):1233-4.
17. Kuru TH, Wadhwa K, Chang RT, et al. Definitions of terms, processes and a minimum dataset for transperineal prostate biopsies: a standardization approach of the Ginsburg Study Group for Enhanced Prostate Diagnostics. BJU International 2013;112(5):568‑77.
18. Vyas L, Acher P, Kinsella J, et al. Indications, results and safety profile of transperineal sector biopsies of the prostate: a single centre experience of 634 cases. BJU International 2014;114(1):32-7.
19. Marra G, Eldred-Evans D, Challacombe B, et al. Pathological concordance between prostate biopsies and radical prostatectomy using transperineal sector mapping biopsies: validation and comparison with transrectal biopsies. Urol Int 2017;99(2):168-76.
20. MacAskill F, Lee SM, Eldred-Evans D, et al. Diagnostic value of MRI-based PSA density in predicting transperineal sector-guided prostate biopsy outcomes. Int Urol Nephrol 2017;49(8):1335-42.
21. Ahmed HU, El-Shater Bosaily A, Brown LC, et al, and the PROMIS study group. Diagnostic accuracy of multi-parametric MRI and TRUS biopsy in prostate cancer (PROMIS): a paired validating confirmatory study. Lancet 2017;389(10071):815-22.
22. Roethke M, Anastasiadis AG, Lichy M, et al. MRI-guided prostate biopsy detects clinically significant cancer: analysis of a cohort of 100 patients after previous negative TRUS biopsy. World Journal of Urology 2012;30(2):213-8.
23. Cormack R, D’Amico A, Hata N, et al. Feasibility of transperineal prostate biopsy under interventional magnetic resonance guidance. Urology 2000;56(4):663‑4.
24. Hata N, Jinzaki M, Kacher D, et al. MR Imaging-guided prostate biopsy with surgical navigation software: device validation and feasibility. Radiology 2001;220(1):263-8.
25. Tempany C, Straus S, Hata N, Haker S. MR-guided prostate interventions. Journal of Magnetic Resonance Imaging 2008;27(2):356-67.
26. Haffner J, Lemaitre L, Puech P, et al. Role of magnetic resonance imaging before initial biopsy: comparison of magnetic resonance imaging-targeted and systematic biopsy for significant prostate cancer detection. BJU International 2011;108(8 Pt 2):E171-8.
27. Rastinehad AR, Turkbey B, Salami SS, et al. Improving detection of clinically significant prostate cancer: magnetic resonance imaging/transrectal ultrasound fusion guided prostate biopsy. The Journal of Urology 2014;191(6):1749-54.
28. Sonn GA, Chang E, Natarajan S, et al. Value of targeted prostate biopsy using magnetic resonance-ultrasound fusion in men with prior negative biopsy and elevated prostate-specific antigen. European Urology 2014;65(4):809-15.
29. Wysock JS, Rosenkrantz AB, Huang WC, et al. A prospective, blinded comparison of magnetic resonance (MR) imaging-ultrasound fusion and visual estimation in the performance of MR-targeted prostate biopsy: the PROFUS trial. European Urology 2014;66(2):343-51.
30. Delongchamps NB, Peyromaure M, Schull A, et al. Prebiopsy magnetic resonance imaging and prostate cancer detection: comparison of random and targeted biopsies. The Journal of Urology 2013;189(2):493-9.
31. Rud E, Baco E, Eggesbo HB. MRI and ultrasound-guided prostate biopsy using soft image fusion. Anticancer Research 2012;32(8):3383-9.
32. Kasivisvanathan V, Rannikko AS, Borghi M, et al. PRECISION Study Group Collaborators. MRI-targeted or standard biopsy for prostate-cancer diagnosis. N Engl J Med 2018;378(19):1767-77.
33. Hansen NL, Barrett T, Kesch C, et al. Multicentre evaluation of magnetic resonance imaging supported transperineal prostate biopsy in biopsy-naïve men with suspicion of prostate cancer. BJU International 2018;122(1):40-49.
34. Jesitus J. MRI guiding future of prostate cancer diagnosis. Urology Times Modern Medicine Network 2014. Available from
http://urologytimes.modernmedicine.com/
urology-times/content/tags/art-rastinehad/
mri-guiding-future-prostate-cancer-diagnosis?page=full.
35. Ganzer R, Brandtner A, Wieland WF, Fritsche HM. Prospective blinded comparison of real-time sonoelastography targeted versus randomised biopsy of the prostate in the primary and re-biopsy setting. World Journal of Urology 2012;30(2):219-23.
36. Brock M, von Bodman C, Palisaar RJ, et al. The impact of real-time elastography guiding a systematic prostate biopsy to improve cancer detection rate: a prospective study of 353 patients. The Journal of Urology 2012;187(6):2039-43.
37. Penzkofer T, Tempany-Afdhal CM. Prostate cancer detection and diagnosis: the role of MR and its comparison with other diagnostic modalities – a radiologist’s perspective. NMR in Biomedicine 2014;27(1):3-15.
38. Braeckman J, Autier P, Garbar C, et al. Computer-aided ultrasonography (HistoScanning): a novel technology for locating and characterizing prostate cancer. BJU International 2008;101(3):293-8.
39. Dundee PE, Grummet JP, Murphy DG. Transperineal prostate biopsy: template-guided or freehand? BJU International 2015;115(5):681-3.
40. DiBianco JM, Mullins JK, Allaway M. Ultrasound guided, freehand transperineal prostate biopsy: an alternative to the transrectal approach. Urology Practice 2016;3(2):134‑40.
41. DiBianco JM, Allaway M. Freehand transperineal prostate biopsy under local anaesthesia. The Journal of Urology 2016;195(4):e466-e467.
42. Kum F, Kulkarni M, Faure-Walker N, et al. The end of transfaecal biopsies: Systematic and targeted prostate biopsies under local anaesthetic in the outpatient setting. BAUS Oncology Section Annual Meeting 2017. Journal of Clinical Urology 2018;11(4):237.
43. Xie L-P, Wang X, Zheng X-Y, et al. A randomized controlled trial to assess and compare the outcomes of AI-US-CT guided biopsy, transrectal ultrasound guided 12-core systematic biopsy, and mpMRI assisted 12-core systematic biopsy. Eur Urol Suppl 2017;16(3):e500.
44. Patel A, Servian P, Winkler M, et al. Robotic MRI/US fusion transperineal biopsy using the iSR’obot Mona Lisa: technique, safety and accuracy. Eur Urol Suppl 2017;16(3):eV42.
45. Bonnal JL, Marien A, Rock A, et al. Trimodal (18) F-choline-PET/mpMRI/TRUS targeted prostate biopsies: first clinical experience. Eur Urol Suppl 2017;16(3):eV49.
46. Pandian S, Madaan S, Sriprasad S. Prostate cancer – Screening & Diagnosis. Annual EAU Congress 2017 – a summary (Urology News Digital Supplement). 2017.













