In the sixth article in this series the authors describe endourology nightmares involving ileal conduits and calculi.
Case 1
A 69-year-old man who had a cystectomy and ileal conduit for muscle invasive bladder cancer, presented with an acute kidney injury secondary to an obstructing 11mm stone proximal to the left uretero-ileal junction (Figure 1). His right kidney was atrophic and poorly functioning. A nephrostomy was placed on the background of chronic renal failure (CKD 3B) with a small improvement in serum creatinine.

Figure 1: Coronal CT demonstrating stone.
A rendezvous procedure was performed. A hydrophilic guidewire was manipulated into the ileal conduit via the nephrostomy and grasped using a cystoscope. A dual lumen ureteric catheter allowed placement of a second antegrade wire. The first was clipped at both ends and used as a safety wire and the second as a working wire. The nephrostomy track was dilated and an 11F/13F ureteric access sheath placed through the kidney down to the stone. Antegrade flexible ureteroscopy was performed and the stone was dusted using laser (Figure 2). A percutaneous stent was placed as the uretero-ileal anastomosis appeared narrowed in addition to a covering nephrostomy.
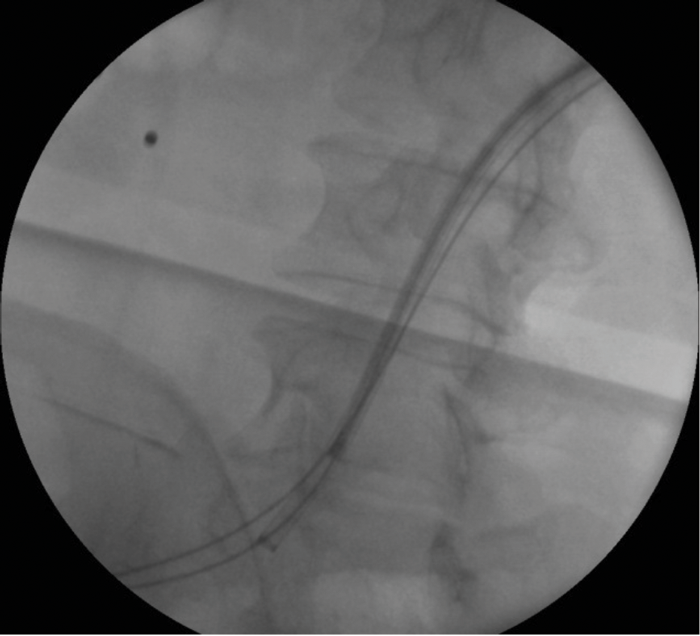
Figure 2: Fluoroscopic image during procedure.
A nephrostogram at one week demonstrated good flow into the conduit and the nephrostomy was removed under fluoroscopic control. The patient presented five days later with the stent visible at the conduit opening (Figure 3). It was re-sited by the interventional radiologist by passing a guide wire through the stent and re-positioning it under fluoroscopy but displaced again a few days later. A subsequent CT confirmed the patient was stone free and the stent was above the level of the uretero-ileal anastomotic stricture. The stent was left in place as the uretero-ileal stricture was the likely cause of the stone forming. A further stent change was planned for three months’ time.
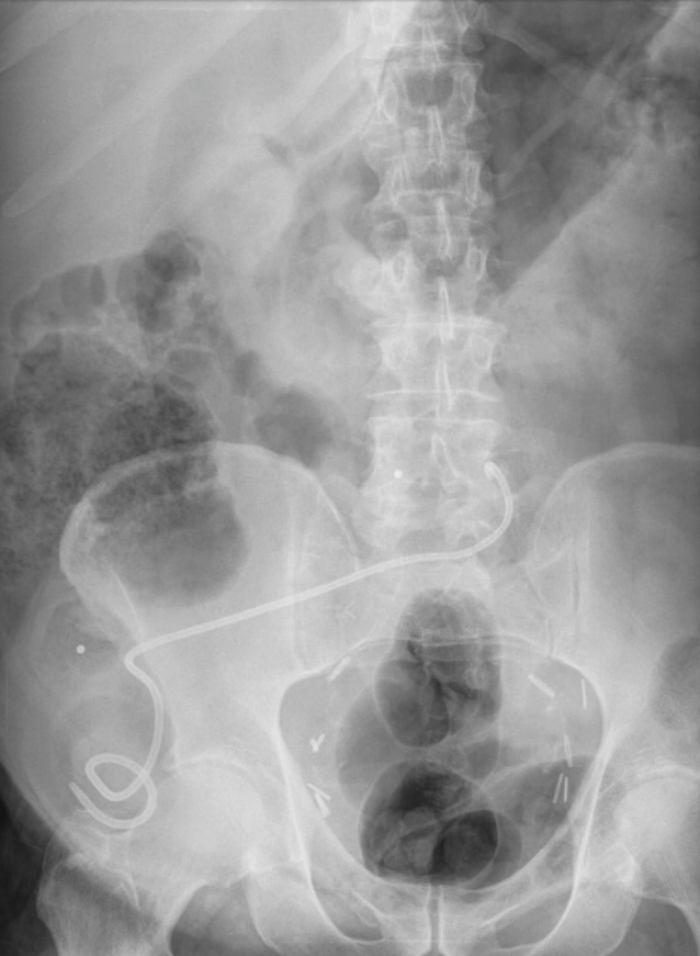
Figure 3: Plain radiograph demonstrating stent migration.
Learning points
-
A rendezvous procedure is a dynamic operation which presents unexpected challenges.
-
Antegrade flexible ureteroscopy is a safe and effective way to manage these stones.
-
Stent migration is much more common in patients with Ileal conduits.
Case 2
A 51-year-old obese patient with spina bifida, epilepsy, left ventricular dysfunction and lifelong warfarin due to a deep vein thrombosis (DVT) had an ileal conduit stone noted as an incidental finding on a CT scan (Figure 1). A 6mm stone was present in the right lower pole. Her urine was colonised with pseudomonas and she was MRSA positive.
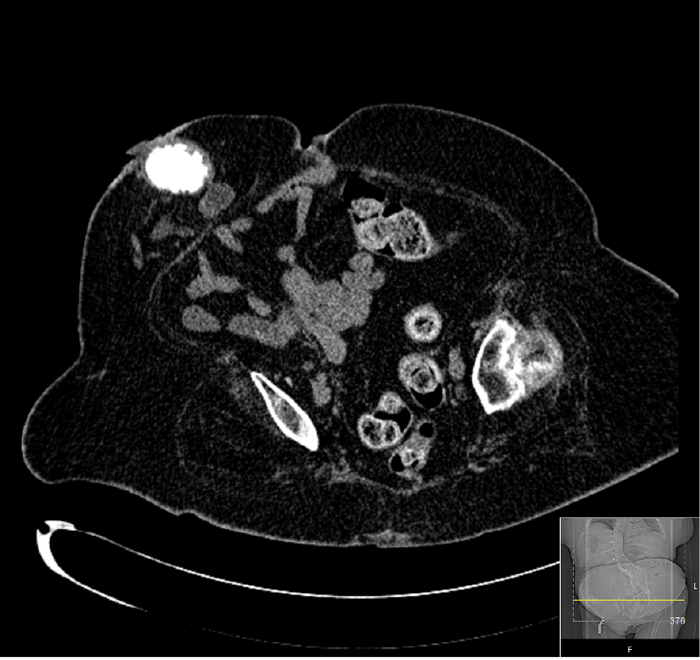
Figure 1: CT scan showing ileal conduit stone.
Under general anaesthesia, a nephroscope was used to fragment the stone in situ which appeared visually clear. This was a technically difficult procedure as the stone was freely mobile in the conduit.
Fragmentation was achieved but a postoperative CT demonstrated a significant residual burden (Figure 2).
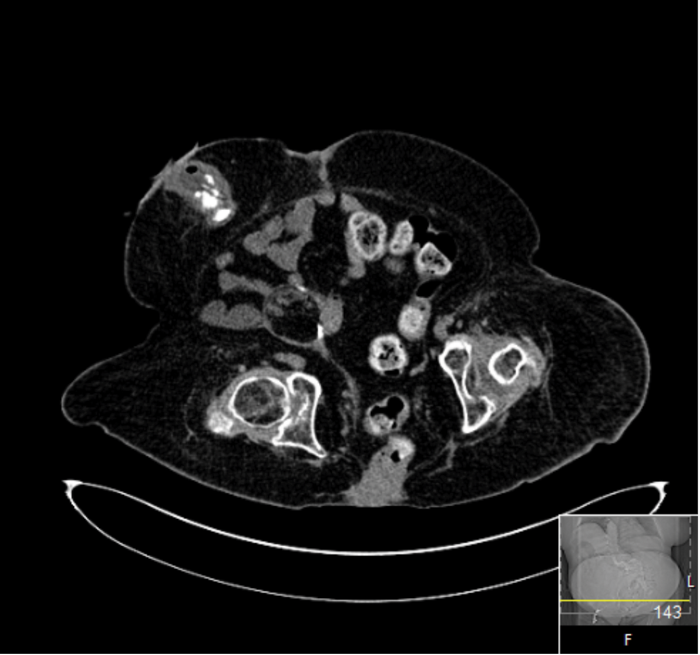
Figure 2: CT scan immediately postoperative.
The patient was lost to short-term follow-up but a three-year CT scan demonstrated her urinary tract to be stone free (Figure 3).
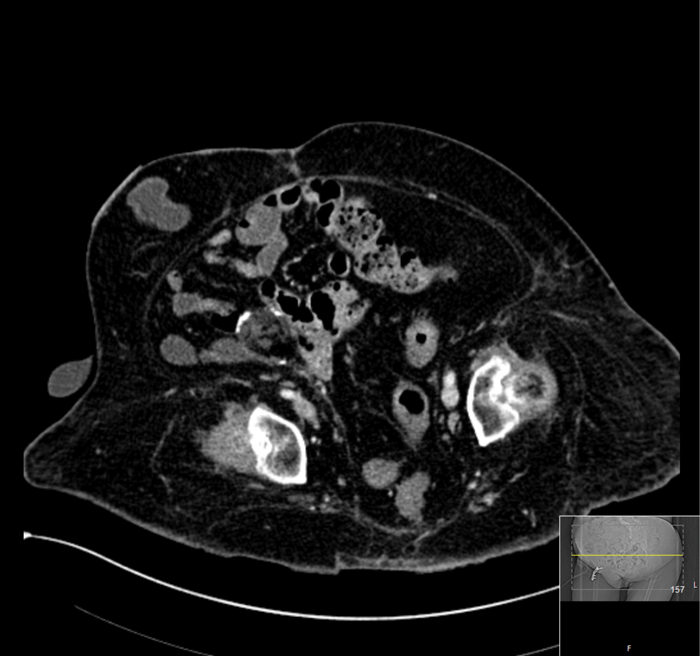
Figure 3: CT scan three years’ postoperative.
Learning points
-
Ileal conduit stones are very rare.
-
Fragmentation is very time-consuming due to the mobility of the stone.
-
Large fragments and indeed upper tract fragments will drain via the conduit.
Email your comments to jennifer@pinpoint-scotland.com




