Partial nephrectomy has become the standard of care in the management of small renal masses. It is a vital tool in maximising nephron preservation and oncological control for patients. It has been shown to produce equivalent oncological outcomes to radical nephrectomy [1,2].
With the introduction of robotic surgery, open surgery is increasingly being used for more complex tumours. Postoperative complications such as pseudoaneurysm and urine leak are well recognised. Distal obstruction leading to urine leak from the kidney is a known issue; however, there have been limited studies into this.
We present a case of a patient who underwent open left partial nephrectomy, where the postoperative recovery was complicated by urine leak secondary to phimosis of the prepuce.

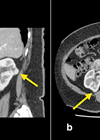
Figure 1: CT (axial and sagittal) views of the renal mass.
Case report
A 69-year-old male with a single left kidney underwent an open left partial nephrectomy for an incidentally diagnosed 5cm left renal mass with possible early collecting system invasion (stage T1b N0 M0) (Figure 1). Prior biopsy showed a papillary renal cell carcinoma type 1. This was found during investigations for episodes of macroscopic haematuria. He was known to have an atrophied right kidney since childhood. He was an ex-smoker (75 pack-year history) and other comorbidities included elevated body mass index (BMI) of 32.5, hypertension, and alcohol excess.
At the time of surgery, he was noted to have a tight foreskin with an unusual appearance. Catheter insertion was challenging, and the foreskin was biopsied. The operation was performed via a supra-12th rib incision and was uneventful. Two renal arteries were identified, and the mass was excised with macroscopically clear margins with a cold ischaemic time of 10 minutes. The collecting system was closed and a two-layered renorrhaphy was performed with no obvious bleeding or urine leak after 30 minutes. Final histopathology showed a 55mm papillary renal cell carcinoma (grade 1), with clear surgical margins, stage pT1b pNx. The foreskin biopsy subsequently showed features consistent with BXO. Postoperative recovery was uneventful, and he was discharged on day six.

Figure 2: CT (axial and coronal) of the pseudoaneurysm and perirenal haematoma.
Ten days postoperative he presented to A&E at another hospital with tachycardia and with fluid leaking from his flank wound. Blood tests showed a Hb drop to 70 (from 100), AKI (eGFR 15), and subsequent CT showed a pseudoaneurysm extending from the posterior aspect with perinephric haematoma and haemoperitoneum (Figure 2). The collecting system was prominent. He underwent urgent angioembolisation with three microcoils injected into the two feeding vessels to the aneurysm, and was transferred to the intensive care unit (ICU). The phimosis was seen to have recurred and caused a degree of urinary retention requiring re-catheterisation.

Figure 3: CT (axial and coronal) showing urinoma (a, b) + persisting pseudoaneurysm (c, d).

Figure 4: Pre- and post- repeat angioembolisation (a, b) and retrograde showing leak at upper pole (c).
In ICU he continued to require blood transfusions, started spiking fevers, and had ongoing fluid leak from his wound. Repeat CT with a delayed phased showed persisting contrast in the aneurysm despite embolisation, and contrast leak from the collecting system (Figure 3). He was transferred to our department and underwent a repeat angioembolisation, retrograde pyelogram and insertion of ureteric stent (Figure 4). A circumcision was also performed, with histopathology confirming lichen sclerosus. He was discharged eight days after transfer, with a plan to remove the urethral catheter and ureteric stent at three weeks and three months respectively.
Discussion
Partial nephrectomy has become the standard of care in the management of T1a and select T1b renal cancers. With the introduction of robotic surgery, it is increasingly being used for more complex and central tumours. It is a vital and imperative nephron-sparing approach for patients with a renal mass in a solitary kidney. Evidence has shown it to have equivalent oncological results to radical nephrectomy, preserve renal function and delay the onset of chronic kidney disease and associated cardiovascular morbidity and mortality [1,2]. Pseudoaneurysm and urine leak are recognised complications of partial nephrectomy [3–5].
Urine leak / urinoma
Risk factors for urine leaks include larger tumour size, endophytic location, entry into collecting system during partial nephrectomy, and age [6]. Management depends on severity, and includes observation, and a combination of ureteric stent, indwelling catheter, nephrostomy, and drain insertion. In more severe cases or those with persistent leak, an open repair or nephrectomy is indicated.
Not commonly investigated in studies, is a urine leak from distal obstruction, which occurred in our case due to phimosis. One study that we identified found five cases of distal obstruction from an anatomical cause. The causes were ureteric stricture, pelviureteric junction (PUJ) obstruction, infundibular stenosis and benign prostatic hyperplasia (BPH) with high pressure voiding [6]. With distal obstruction, the identified studies all agree that intervention to relieve the obstruction is required [6,7]. This was in the form of stent, catheter, and drain. However, even though a shorter recovery period was noted, the duration of stent and drainage was variable, ranging from 45 to 105 days [8,9].
Phimosis / lichen sclerosus and bladder outlet obstruction
Phimosis can be classified as physiological or pathological. Pathological phimosis requires intervention. Lichen sclerosis is a progressive, inflammatory condition of the glans penis and foreskin leading to discolouration, and scarring, where pathogenesis is not completely understood [10].
Complications of phimosis and lichen sclerosus include balanoposthitis, painful erections, meatal stenosis, urethral strictures, and penile cancer. In severe cases it can cause similar complications to bladder outlet obstruction such as retention, high pressure voiding, and obstructive uropathy [11]. Interventions, such as circumcision or urethral dilatation, are required in such situations, to prevent these complications.
As a result, all men undergoing partial nephrectomy should be examined preoperatively for phimosis / meatal stenosis and questioned about symptoms of bladder outflow obstruction prior to the operation. If significant bladder outflow obstruction is identified this should be managed prior to the partial nephrectomy or simultaneously if time critical.
In this case, the urine leak was caused by lower tract obstruction due to a number of factors. The patient had reported some lower urinary tract symptoms (LUTS) prior to the procedure. This was relieved whilst catheterised, and returned after removal of the catheter, with subsequent urine leak. After intervention was performed on the lower tract, his symptoms improved, and there were no further issues with leakage after this.
Conclusion
Partial nephrectomy is an important nephron-sparing procedure that is increasing in use. With the introduction of robotic surgery, it is increasingly being used in more complex patients and tumours. Vital to postoperative recovery is a full preoperative assessment for bladder outflow obstruction.
To avoid or minimise postoperative complications, it is important to properly investigate, assess, and treat lower urinary tract pathology before upper tract interventions, such as partial nephrectomy and pyeloplasty.
References
1. Huang WC, Level AS, Serio AM, et al. Chronic kidney disease after nephrectomy in patients with renal cortical tumours: a retrospective cohort study. Lancet Oncol 2006;7(9):735–40.
2. Zini L, Perrotte P, Capitàni U, et al. Radical versus partial nephrectomy: effect on overall and noncancer mortality. Cancer 2009;115(7):1465–71.
3. Albani JM, Novick AC. Renal artery pseudo aneurysm after partial nephrectomy: three case reports and a literature review. Urology 2003;62(2):227–31.
4. Fergany AF, Saad IR, Woo L, et al. Open partial nephrectomy for tumor in a solitary kidney: experience with 400 cases. J Urol 2006;175(5):1630–3.
5. Inderbir SG, Kavoussi LR, Lane BR, et al. Comparison of 1,800 laparoscopic and open partial nephrectomies for single renal tumors. J Urol 2007;178(1):41–6.
6. Meeks JJ, Zhao LC, Naval N, et al. Risk factors and management of urine leaks after partial nephrectomy. J Urol 2008;180(6):2375–8.
7. Erich T, Abu-Ghanem Y, Ramon J, et al. Postoperative urinary leakage following partial nephrectomy for renal mass: risk factors and a proposed algorithm for the diagnosis and management. Scand J Surg 2017;106(2):139–44.
8. Ramani AP, Desai MM, Steinberg AP, et al. Complications of laparoscopic partial nephrectomy in 200 cases. J Urol 2005;173(1):42–7.
9. Simmons MN, Gill IS. Decreased complications of contemporary laparoscopic partial nephrectomy: Use of a standardized reporting system. J Urol 2007;177(6):2067–73.
10. Powell JJ, Wojnarowski F. Lichen sclerosus. Lancet 1999;353:1777–83.
11. Singh JP, Priyadarshi V, Gole HK, et al. Penile lichen sclerosis: an urologist’s nightmare! A single centre experience. Urol Ann 2015;7(3):303–8.
Declaration of competing interests: None declared.